All published articles of this journal are available on ScienceDirect.
Attachment in Patients with Bipolar and Unipolar Depression: A Comparison with Clinical and Non-clinical Controls
Abstract
Background:
A link between depression and insecure attachment has long been postulated. Although many studies examined the relationship between depressive symptoms and attachment, relatively few studies were performed on patients diagnosed with depression. Also, research on patients with bipolar disorder is scarce.
Objective:
We aimed at testing the association between attachment insecurity and unipolar and bipolar depression.
Methods:
We studied 21 patients with bipolar disorder, current episode depressed, and three age- and sex-matched groups, each consisting of 21 individuals: patients with major depressive disorder, recurrent episode; patients with epilepsy; non-clinical participants. The Experience in Close Relationships questionnaire was used to assess adult attachment style.
Results:
Patients with both bipolar and unipolar depression displayed significantly higher scores on attachment-related avoidance as compared with patients with epilepsy and non-clinical participants. Also, patients with bipolar depression scored significantly higher on attachment-related anxiety than all other groups. In both psychiatric groups, attachment dimensions were not significantly correlated with global clinical severity or severity of depression.
Conclusion:
Despite some study limitations, our results are consistent with some previous studies and provide support to Bowlby's seminal hypothesis that attachment insecurity may predispose to depression. Attachment theory may provide a valuable theoretical framework for future research and for guiding treatment.
1. INTRODUCTION
Depression is a major public health concern. Major depressive disorder and bipolar disorder are quite prevalent in the general population [1] and together account for 3% of the world’s disease burden [2].
A variety of biological, social, and psychological factors contribute to the development of depression [3-5]. One of the most consistently identified risk factors is family history. Studies using genetically informative designs reported both substantial heritability and significant environmental effects [6-8], which corroborates the view that family environment factors increase vulnerability to mood disorders.
Given that attachment security is strongly related to early life experiences in the family, attachment may be hypothesised to play a role in shaping individual vulnerability to depression. Indeed, attachment plays a major part in the development of emotion regulation [9] and models of self [10], and there are important links between depression, dysfunctional emotion regulation [11], and dysfunctional schemas about the self [12].
Attachment theory [13-15] is a life-span developmental theory that postulates that humans have the disposition to build and maintain some intimate social bonds that are critical for survival and good health. The term “attachment” refers to the emotional, cognitive, and behavioural processes involved in the formation and preservation of these bonds. Attachment bonds are first formed with parents. These bonds are maintained across childhood and into adulthood, although from adole- scence onwards committed romantic relationships progres- sively become the primary attachment bond for each person [16, 17].
According to attachment theory, children develop internal working models of self and others on the basis of early interactions and experiences with their caregivers. These models shape their expectations of how their future relational interactions will play out and also shape the associated emotional and behavioural responses [13]. The term “attach- ment style” is used to indicate individual differences in emotion regulation, patterns of relating to significant others, beliefs about self and significant others, and the way significant others are perceived. Research suggests that there are two major dimensions underlying adult attachment style, i.e., attachment-related anxiety and avoidance. The first refers to the fear of being abandoned or not loved enough, the second to discomfort with intimacy and the expression of emotions [17]. Interestingly, the behaviour of infants during Ainsworth’s “Strange Situation” [18] can be mapped onto two conceptually similar dimensions [19]. Also, these dimensions show theore- tically consistent correlations with the Big Five personality traits, temperament, character, coping, self-esteem, self-efficacy, verbal intelligence, social desirability, physical attrac- tiveness, and relationship satisfaction [20-22].
Low to moderate levels of both attachment-related anxiety and avoidance characterise secure attachment patterns. In romantic relationships, secure individuals tend to see them- selves as valued and worthy of affection, and their partners as trustworthy, reliable, and available to provide support. Individuals with elevated attachment-related anxiety are characterised by a “hyper-activation” of the attachment system; they are prone to preoccupation with their romantic relation- ships and are inclined to feel underappreciated and to worry about being insufficiently loved or abandoned. Individuals with high attachment-related avoidance are characterised by a “deactivation” of the attachment system; they find it difficult to trust or depend on their partner, are unwilling to ask for support, and prefer to maintain emotional distance [17].
In his seminal work, Bowlby proposed a link between depression and attachment [14]. His ideas have subsequently received empirical support from investigations on the long-term effects of adverse attachment-related experiences (e.g., the death of or prolonged separation from a parent in early childhood) on the risk of developing depression later in life. Also, many studies performed on non-clinical samples reported that the security of attachment to parents or peers, secure states of mind with regard to attachment, and endorsement of a secure attachment style in close relationships are related to lower levels of depressive symptoms [17, 23].
However, relatively few studies were performed on clinical samples of adolescent and adult patients with a diagnosis of depression. Most of these investigations involved patients with unipolar depression. While they have consistently reported an association between unipolar depression and attachment insecurity [24-34], the findings are less consistent regarding the type of insecurity that mostly characterises these patients. Some studies reported that depression was associated with preoccupied states of mind about attachment [26, 34], or that it is attachment anxiety that mostly characterises depression [30, 32]. Other studies reported that depression was associated more closely with dismissing states of mind [28, 31], or highlighted an increase in both anxiety and avoidance [29, 33]. The few studies performed on patients with bipolar disorder have consistently reported higher attachment insecurity in these patients as compared with healthy controls [27, 29, 35-38]. However, inconsistent findings have emerged regarding the type of insecurity that mostly characterises these patients [35, 37] and from studies comparing bipolar with unipolar depression [26, 27, 29, 38].
While the studies performed so far corroborate an association between attachment and depression, the scarcity of research on patients with bipolar disorder represents an important gap in the literature [39]. Also, the findings are inconsistent regarding the type of insecurity that mostly characterises unipolar and bipolar depression. Furthermore, many studies were hampered by methodological limitations, such as the use of less sophisticated measures of attachment, reliance on clinical diagnoses not confirmed by standardised psychiatric interviews, and lack of control for possible confounding by demographic characteristics, current mood state, or presence of a long-term illness.
We aimed at further testing the hypothesis that attachment insecurity is increased in patients with bipolar and unipolar depression as compared with non-depressed individuals, and at investigating whether there are differences in attachment style between patients with bipolar and unipolar depression. To this purposes, we used validated measures to assess adult attachment style and to establish psychiatric diagnosis, while controlling for demographic characteristics by matching the study groups for age and sex; for current mood state by including in the bipolar and unipolar patient groups only patients who were experiencing a major depressive episode; and for the presence of a long-term illness by including as non-psychiatric comparison groups both a non-clinical group and a group of patients with epilepsy.
2. METHODS
2.1. Participants
The patients with bipolar depression were recruited in the inpatient ward and the outpatient clinic of the psychiatric department of the Umberto I Policlinico Hospital, Sapienza University of Rome, and in a private psychiatric facility situated in the same city. All adult patients of Italian nationality, with no major medical disease or cognitive impairment, who were consecutively admitted to these units over a two-year period and received a diagnosis of bipolar I or II disorder, current episode depressed, were invited to take part in the study. The study was carried out in accordance with the Ethical Code of Conduct of the Italian National Institute of Health with written informed consent from all participants. According to the Italian legislation, purely observational, cross-sectional studies based on data collected as part of routine patient assessment do not need formal ethical approval. However, we decided to still obtain written informed consent from all participants according to the International Ethical Guidelines for Biomedical Research Involving Human Subjects and the Declaration of Helsinki.
Within three days from admission, the participants were administered the Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I) [40] to establish the diagnosis, the 24-item version of the Brief Psychiatric Rating Scale [41], and the Experience in Close Relationships questionnaire (ECR) [19].
Three comparison groups were selected. In each group, participants were individually matched to patients with bipolar disorder for sex and age. The first group included patients with major depressive disorder, recurrent episode, who were recruited with the same procedure at the same sites as the patients with bipolar depression, and were administered the same assessment instruments. All of them signed written informed consent to take part in the study.
The second group was recruited among friends and relatives of a number of physicians attending as graduate students the Department of Neurology and Psychiatry, Policlinico Umberto I Hospital, Sapienza University of Rome, Italy. It was a standard non-clinical control group, consisting of individuals who were free from cognitive impairment and severe medical or psychiatric illness as clinically determined. They completed the ECR after giving their written informed consent to take part in the study.
Also, in order to control for the presence of chronic illness, long-term medication treatment, and hospitalization, we included a third comparison group, which included inpatients with drug-resistant epilepsy. They completed the ECR as part of a multidisciplinary presurgical assessment protocol including psychiatric evaluation at the Epilepsy Surgery Unit of the Neuromed-IRCCS Neurological Institute, situated in Pozzilli, about 100 miles east from Rome. Although some patients had depressive or anxiety symptoms, none of them was experiencing a major depressive episode. All patients gave their written informed consent to take part in the study. As such patients are usually young, perfect age matching could not be accomplished. While the age matching was very close for the other two comparison groups, differences of up to 10 years had to be allowed for patients with drug-resistant epilepsy; however, they did not significantly differ in mean age from the other study groups and were close enough in age to provide a good matching.
Table 1 summarises the clinical and demographic characteristics of all study participants.
| - | Bipolar depression | Recurrent major depression | Drug-resistant epilepsy | Non-clinical subjects | ||||
|---|---|---|---|---|---|---|---|---|
| - | N (%) | Mean ± SD | N (%) | Mean ± SD | N (%) | Mean ± SD | N (%) | Mean ± SD |
| Sex | - | - | - | - | - | - | - | - |
| Male | 11 (52.4) | - | 11 (52.4) | - | 11 (52.4) | - | 11 (52.4) | - |
| Female | 10 (47.6) | - | 10 (47.6) | - | 10 (47.6) | - | 10 (47.6) | - |
| Age | - | 54.1 ± 10.9 | - | 53.2 ± 11.7 | - | 47.8 ± 7.8 | - | 53.3 ± 9.6 |
| Education | - | - | - | - | - | - | - | - |
| Primary school | 0 (0.0) | - | 3 (14.3) | - | 0 (0.0) | - | 0 (0.0) | - |
| Junior high school | 6 (28.6) | - | 5 (23.8) | - | 6 (28.6) | - | 3 (14.3) | - |
| Senior high school | 11 (52.4) | - | 12 (57.1) | - | 9 (42.8) | - | 12 (57.1) | - |
| University degree | 4 (19.0) | - | 1 (4.8) | - | 4 (19.0) | - | 6 (28.6) | - |
| Marital status | - | - | - | - | - | - | - | - |
| Unmarried | 5 (23.8) | - | 5 (23.8) | - | 3 (14.3) | - | 3 (14.3) | - |
| Married | 10 (47.6) | - | 8 (38.1) | - | 15 (71.4) | - | 13 (61.9) | - |
| Separated or divorced | 6 (28.6) | - | 6 (28.6) | - | 1 (4.8) | - | 3 (14.3) | - |
| Widowed | 0 (0.0) | - | 2 (9.5) | - | 1 (4.8) | - | 1 (4.8) | - |
| Diagnosis | - | - | - | - | - | - | - | - |
| Bipolar I disorder, current episode depressed | 13 (61.9) | - | - | - | - | - | - | - |
| Bipolar II disorder, current episode depressed | 8 (38.1) | - | - | - | - | - | - | - |
| Major depressive disorder, recurrent episode | - | - | 21 (100.0) | - | - | - | - | |
| Drug-resistant epilepsy | - | - | - | 21 (100.0) | - | - | - | |
| No severe medical or psychiatric illness | - | - | - | - | - | - | 21 (100.0) | - |
| BPRS total score | - | 41.1 ± 9.7 | - | 45.4 ± 10.5 | - | - | - | - |
2.2. Assessment Instruments
The ECR questionnaire [19] is a validated measure of adult attachment style that has been used extensively by researchers in several countries to investigate links between attachment insecurity and a variety of correlates including genetic polymorphisms related to emotions and social behaviour [42], immune function [43, 44], brain activity [45] and structure [46], and vulnerability to physical [47, 48] and mental [29, 49, 50] health problems. The ECR displayed measurement invariance across a variety of clinical and non-clinical populations [51], and been shown to provide a sufficiently reliable assessment of attachment style not only in healthy or mildly or moderately distressed individuals, but also in psychiatric inpatients, even those diagnosed with a psychotic disorder, except for the most severely impaired patients [52]. It is a self-report instrument consisting of 36 items, each scored on a seven-point scale. The ECR yields scores on two scales, called ‘Anxiety’ and ‘Avoidance’, each consisting of 18 items, some of which are reverse-keyed. Higher scores indicate greater insecurity. Individuals scoring high on Anxiety tend to be preoccupied with romantic relationships, to worry about being abandoned, to desire a high degree of closeness, and to ask the partner for more commitment. Individuals scoring high on Avoidance tend to maintain emotional distance and avoid intimacy, are uncomfortable depending on their partner, and are reluctant to ask for support. We used the validated Italian version of the instrument [53]. In this study, the reliability of the ECR scales as measured by Cronbach’s Alpha coefficient was 0.86 and 0.85 for Anxiety and Avoidance, respectively.
Psychiatric diagnoses were made by trained clinicians using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I) [40]. Several studies provided evidence of the superior validity of this clinician-administered interview over routine clinical interviews [54, 55].
Clinical severity was evaluated by means of the 24-item version of the BPRS [41], which is a clinician-rated instrument consisting of 24 items, scored on a 7-point severity scale. We used a validated Italian version, which has high reliability [56] and is based on the BPRS manual of administration, with defined anchor points and detailed probe questions and rules for scoring [57]. The items are scored on a 7-point severity scale ranging from 1 to 7. Higher scores indicate greater severity of psychiatric symptoms.
The clinicians who administered the SCID-I and the BPRS received specific training in administering and scoring the instruments. They based their ratings on all sources of information available, including not only patients’ answers and clinical observation, but also referral notes, medical records, and reports by relatives and friends. The inter-rater reliability was assessed on several occasions during the study period. The reliability of the SCID-I as measured by the kappa coefficient was satisfactory as it ranged from .75 to .94 for the most common diagnoses (psychotic, mood, anxiety, and eating disorders). The mean inter-rater reliability of the BPRS as measured by the intraclass correlation coefficient was also satisfactory, as it ranged from .85 to .93.
2.3. Statistical Analysis
Given that the previous literature consistently suggested substantial differences in attachment security between depressed patients and non-psychiatric controls, it would be reasonable to expect a medium to large effect size. A sensitivity analysis using G-power software, version 3.1 [58] indicated that, given alpha of 0.05 and power (1-beta) of 0.80, a study with four groups and a total sample size of 84 would be able to detect an effect size of 0.37 with a fixed effects, omnibus, one-way ANOVA (noncentrality parameter lambda = 11.44; critical F = 2.71; numerator df = 3; denominator df = 80). Therefore, the study is sufficiently powered to detect moderate differences in ECR scores between groups.
All statistical analyses were performed using SPSS Statistics for Mac, Version 20 (IBM Corp., Armonk, NY, USA). All statistical tests were two-tailed, with alpha set at 0.05. Firstly, participant characteristics were summarized using appropriate descriptive statistics. Then, Pearson’s correlation coefficient was used to test for the association between continuous variables, and the Chi-square test or Fisher’s exact test and analysis of variance (ANOVA) were used as appropriate to test for differences between groups in categorical or continuous variables, respectively. In order to adjust for multiple comparisons in ANOVA, Tukey’s post-hoc test was used for pairwise comparisons between groups.
3. RESULTS
On the one hand, as a result of the matching procedure, there were no significant differences in age, marital status, educational level, and BPRS scores between the study groups.
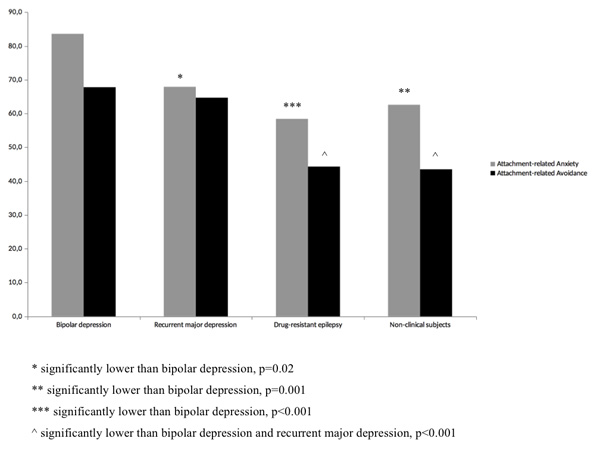
On the other hand, as illustrated in Fig. (1), ANOVA revealed several significant between-group differences in attachment dimensions. The omnibus ANOVA was highly significant for both attachment-related anxiety (F = 8.33, df = 3, 80) and attachment-related avoidance (F = 14.15, df = 3, 80). Tukey’s post hoc test revealed that both patients with bipolar depression and recurrent major depression scored significantly higher (p<0.001) on attachment-related avoidance (mean scores 67.8±13.0 and 64.7±14.6, respectively) than patients with epilepsy and non-clinical controls (mean scores 44.3±21.8 and 43.5±11.9, respectively). The effect size of these differences was high (Cohen’s d = 1.31 with 95% C.I. 0.36-2.25 for the comparison between bipolar disorder and epilepsy; 1.95 with 95% C.I. 0.91-2.98 between bipolar disorder and non-clinical controls; 1.10 with 95% C.I. 0.18-2.01 between major depressive disorder and epilepsy; 1.59 with 95% C.I. 0.61-2.57 between major depressive disorder and non-clinical controls). Also, Tukey’s post hoc test showed that patients with bipolar depression scored significantly higher on attachment-related anxiety (mean score 83.6±12.5) as compared with patients with recurrent major depression (mean score 67.9±14.8; p=0.02), patients with epilepsy (mean score 58.4±22.3; p<0.001) and non-clinical controls (mean score 62.6±18.7; p=0.001). The effect size of these differences was high, too (Cohen’s d = 1.14 with 95% C.I. 0.22-2.06 for the comparison between bipolar disorder and major depressive disorder; 1.39 with 95% C.I. 0.44-2.34 between bipolar disorder and epilepsy; 1.32 with 95% C.I. 0.37-2.26 between bipolar disorder and non-clinical controls). The patients with recurrent major depression displayed higher scores on attachment-related anxiety (mean score 67.9±14.8) than the non-psychiatric control groups (mean score 58.4±22.3 and 62.6±18.7 for patients with epilepsy and non-clinical participants, respectively); while these between-groups differences were in the expected direction, they were of moderate magnitude (Cohen’s d = 0.50 with 95% C.I. -0.36-1.37 for the comparison between major depressive disorder and epilepsy; 0.31 with 95% C.I. -0.54-1.17 between major depressive disorder and non-clinical controls) and did not reach statistical significance.
There were no significant differences in attachment-related anxiety and avoidance between patients with bipolar I and bipolar II disorder. Also, no significant association between attachment dimensions and age, sex, marital status, or education was found in any group, except the findings of higher attachment-related anxiety in women as compared with men in the epilepsy group. In both psychiatric groups, attachment dimensions were not significantly correlated either with global clinical severity as measured by the BPRS total score, or with the severity of depression as measured by relevant BPRS items, such as depression, anxiety, suicidality, and guilt (all p>0.10).
4. DISCUSSION
The theoretical links between attachment insecurity and depression were first formulated by Bowlby [14]. He suggested that the loss of attachment security in early life contributes to the development of depression in adulthood, because the loss of security promotes the formation of negative representations of self and the world. Loss of attachment security can result not only from the death of a primary caregiver, but also from repeated failures to establish a secure relationship with a caregiver. A child who, despite may attempts, is unable to create stable and secure relationships with caregivers, tends to develop a model of the self as unworthy and incompetent, as he or she is likely to feel powerless and helpless in trying to keep a neglectful parent present, or to gain support, love, and approval from an inconsistently responsive or rejecting parent. Also, a child who consistently receives the message from a parent that he or she is incapable of inspiring love or admiration tends to form a model of the self as unlovable and a complementary model of others as unloving [59].
Consistently with theoretical expectations, we found that patients with unipolar and bipolar depression were character- ised by higher levels of attachment insecurity as compared with non-psychiatric comparison groups. Among attachment dimen- sions, it was avoidance that mostly distinguished depressed patients from controls. On the one hand, both patients with bipolar depression and recurrent major depression displayed significantly higher scores on attachment-related avoidance than patients with epilepsy and non-clinical participants, with differences of large magnitude. On the other hand, the difference in attachment-related anxiety between patients with unipolar depression and the non-psychiatric control groups was moderate in magnitude and did not reach statistical signi- ficance. This finding is consistent with theoretical formulations suggesting that consistent rejection and neglect by the caregiver, which are the postulated antecedents of avoidant attachment, may lead a child to form an internal working model of himself or herself as not worthy of help and comfort [59], which would predispose to depression [60]. This finding is also in line with previous studies reporting that unipolar depression was associated more closely with dismissing states of mind about attachment [28, 31] and that patients with bipolar disorder were more often characterised by an avoidant attachment style as compared with healthy controls [35]. However, the literature is not consistent regarding the type of insecurity that is more prevalent in depressed patients. Some studies using interview measures of attachment reported that depression was associated with preoccupied states of mind about attachment [26, 34]. Also, some of the studies using self-report instruments that allow distinguishing anxious from avoidant attachment features suggested that it is attachment anxiety that mostly characterises depression [30, 32], while others reported an increase in both anxiety and avoidance [29, 33]. Differences between studies in design, assessment instrument, specific depressive disorder studied, psychiatric comorbidity, and predominance of externalising or internal- ising symptoms [23] may account for the discrepancies in findings.
This finding of higher attachment insecurity in depressed patients is unlikely to be explained by mood state, as depressive symptoms do not substantially affect ECR scores. In a study on non-clinical participants, ECR scores showed only a modest correlation with depressive symptoms [22]. In a study on psychiatric inpatients, ECR scores did not significantly correlate with the severity of depressive symptoms at admission, and they showed high absolute and relative stability over a 2-month interval despite a substantial improvement in depressive symptoms during inpatient stay [52]. The finding of greater attachment insecurity in patients with depression is also unlikely to be explained by a sedative or antidepressant medication. Although the effect of psychotropic drugs on attachment measures has not been formally tested, if there is any effect it is likely in the direction of reducing perceived insecurity, which would actually attenuate the difference with non-psychiatric control groups. Our finding corroborates previous reports of greater attachment insecurity in patients with unipolar [24, 27-30, 32, 33] and bipolar [27, 35-38] depression as compared with healthy controls. The present study also extends previous findings by showing that attachment insecurity in depression is also higher than in a severe chronic neurological disease, such as drug-resistant epilepsy.
Attachment insecurity, in itself, is unlikely to be a sufficient cause of mood disorders. Other biological, psycho- logical, and socio-cultural factors are likely to complement or potentiate the effects of attachment experiences in the development of psychopathology [61]. While keeping this in mind, research has started to reveal some pathways through which attachment insecurity can contribute to vulnerability to depression. The findings implicate a network of interrelated cognitive, coping, and interpersonal processes by which attachment insecurity may increase susceptibility to depression. Concerning cognitive processes, the negative attitudes rooted within the internal working models of insecurely attached individuals may negatively bias perceptions of the self and of close relationship partners [62]. Indeed, research suggests a mediating role for low self-esteem, low self-efficacy expec- tancies, threat appraisal, perceived lack of social support, maladaptive perfectionism, self-criticism, and hopelessness [17, 27]. Regarding emotion regulation, attachment theory posits that secure individuals develop healthy emotion regulation skills through interactions with available caregivers. On the contrary, individuals with high attachment anxiety or avoidance tend to rely on emotion regulation strategies that amplify or suppress emotion, respectively. Research indeed indicates that difficulties in emotion regulation may contribute to the link between insecure attachment and mood disorders [17, 63]. As far as interpersonal processes are concerned, the repeated failure to receive support from caregivers and the resulting reliance on insecure strategies based on the hyper-activation or deactivation of the attachment system hinder the acquisition of social skills and cause substantial problems in interpersonal relations. Indeed, research suggests that interpersonal difficulties, such as reduced emotional expressiveness, difficulties with assertiveness, excessive reassurance seeking, inability to meet closeness and autonomy needs, and feelings of loneliness, act as additional mediating paths between attachment insecurity and mood disorders [17].
It has also been hypothesised that the decreased ability to feel soothed and safe with attachment figures that characterises insecure attachment may predispose individuals to an increased focus on and concern for social rank. Insecurely attached individuals may tend to rely more on social competition strategies than affiliative strategies in order to achieve a place in the social group that allows them to exercise control over social resources [64]. The interaction between attachment and social rank systems might be particularly relevant in bipolar disorder, as mood variation was found to be linked to variation in social rank evaluations in patients with bipolar disorder [65], while mania proneness was found to be related to the pursuit of dominance and socially dominant behaviours [66].
In this study, the group showing the highest level of attachment insecurity was the group of patients with bipolar depression. These patients displayed significantly higher scores on attachment-related avoidance than non-psychiatric controls, and showed significantly higher scores on attachment-related anxiety not only compared with non-psychiatric controls, but also with patients with unipolar depression. This finding suggests the presence, at least in some patients, of a fearfully avoidant attachment style. Fearful avoidance is characterised by high levels of both anxiety and avoidance and has some degree of overlap with the construct of disorganized attachment [67, 68]. Theoretically, fearful avoidance derives from a failure to attain any of the objectives of the three main attachment strategies, i.e., protection and support resulting from proximity seeking, or intense and chronic activation of the attachment system until proximity is achieved, or defensive deactivation of the system. This can happen if a child is abused, or if he or she has a confused, drug-addicted, or grieving parent, whose behaviour cannot be predicted and who cannot be relied upon to provide comfort. In such cases, the attachment system is reactivated despite deactivating strategies, attachment-related needs and worries become simultaneously accessible, and the child gets trapped in a cycle of conflict-riddled attempts to meet personal needs while avoiding rejection or mishandling. Research indicates that fearfully avoidant individuals have especially negative representations of their romantic partners, are more likely than others to be involved in highly distressed and violent couple relationships, and have the poorest mental health [17]. Given their difficulty developing a coherent attachment strategy and the related severe deficits in emotion and behaviour regulation, these individuals may also experience rapid shifts between states of hyper-arousal and withdrawal, which may result in disorganisation of affects and associated behaviours [69] and in the development of mood instability, thereby increasing their vulnerability to bipolar disorder. Childhood traumatic experiences, particularly emotional neglect, appear indeed to be significantly associated with bipolar disorder [70]. Of note, childhood trauma may interact with a number of genes involved in a variety of biological pathways to decrease the age of onset of the disorder or increase suicide risk. Epigenetic molecular mechanisms may also play a role in the neurobiological effects of childhood trauma in bipolar disorder [71].
Strong points of this study are the use of state-of-the-art instruments to establish a psychiatric diagnosis and measure adult attachment style, the inclusion of multiple clinical and non-clinical comparison groups, and the use of individual matching for demographic variables to control confounding. However, the study has also several limitations. Firstly, the sample size was relatively small, although the study was sufficiently powered to detect medium to large between-group differences. Secondly, the cross-sectional design precludes firm causal inferences regarding the nature of relationships between variables. Although there is evidence of moderate stability of individual differences in attachment security from infancy to adulthood [72, 73], it cannot be stated with certainty that the high levels of insecurity that we observed in our patients were already present during childhood and predated the onset of their mood disorder. Thirdly, it cannot be ruled out that the insecurity displayed by our patients with mood disorders may at least partly follow from experiencing long-term illness. This limitation is inherent in the long-term nature of the disorders in question, as a substantial period of time is required before the diagnosis can be made. However, the inclusion of a comparison group consisting of patients suffering from a chronic illness in which depressive and anxiety symptoms are common [74] should mitigate this limitation. Fourthly, we used a self-report measure to assess adult attachment. Despite being valid and reliable, self-report measures of romantic attachment cannot be considered identical to interview measures of the state of mind with regard to attachment experiences during childhood [75]. Further studies are needed to extend our findings to interview measures of attachment. Fifthly, although no participant included in the non-psychiatric control groups was experiencing a major depressive episode, we cannot exclude that depressive symptoms were present to some degree in a number of these participants. However, this would not threaten the validity of our findings, as it would have had a conservative effect on the results. Sixthly, our findings may not generalise to patients with other forms of unipolar depression, such as single episode major depression or dysthymic disorder. Seventhly, some degree of selection bias may have occurred as attachment style may affect help-seeking behaviour, including the decision to seek treatment. A further limitation is that we relied on a single assessment; a follow-up evaluation would have been useful to confirm the results. Finally, we did not measure putative mediators of the association between insecure attachment and mood disorders, such as cognitive vulnerability factors, impaired emotion regulation, and interpersonal difficulties.
CONCLUSION
Although these limitations suggest a cautious interpretation of the results, they are consistent with previous studies and support Bowlby's hypothesis that attachment insecurity may predispose to depression [14]. Attachment theory also provides a valuable framework for guiding treatment. Authors from several different theoretical perspectives [76-81] have delineated several ways in which attachment theory can help inform clinical practice and therapeutic interventions. These principles can be applied not only to psychotherapy for unipolar depression, but also to psychotherapeutic interven- tions for bipolar disorder involving both patients and their relatives, such as family-focused treatment [82] and cognitive-psychoeducational group interventions [83]. Interventions specifically addressing the attachment and affiliative systems in patients with bipolar disorder are also being developed [84]. Also, attachment theory provides a helpful framework for informing the design and delivery of general mental health services in order to meet users’ attachment needs [85]. In the field of mood disorders, research based on attachment theory is still relatively scarce, and several important issues need to be addressed. Firstly, longitudinal studies are needed to confirm the role of attachment insecurity as a risk factor for mood disorders. Secondly, more research is necessary on the relationship between specific attachment dimensions and patterns and different forms of mood disorders. Thirdly, there is a need for controlled clinical trials examining the effectiveness of attachment-informed interventions in improving the outcome for patients with mood disorders. Finally, future studies should investigate the interaction between insecure attachment and other risk factors, including both genetic and environmental influences.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was carried out in accordance with the ethical code of conduct of the Italian National Institute of Health.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. The study protocols were followed in accordance with the international ethical guidlines for biomedical research involving human subjects and the declaration of helsinki.
CONSENT FOR PUBLICATION
Written and informed consent was obtained from all the participants.
AVAILABILITY OF DATA AND MATERIAL
The study dataset cannot be placed in a public repository as this would violate the Italian privacy law, even if the data were anonymized. Interested researchers may request the data to the corresponding author.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


