RESEARCH ARTICLE
Built Environment and Elderly Population Health: A Comprehensive Literature Review
Noe Garin 1, 2, 3, Beatriz Olaya 1, 2, 3, Marta Miret 3, 4, 5, Jose Luis Ayuso-Mateos 3, 4, 5, Michael Power 6, Paola Bucciarelli 7, Josep Maria Haro *, 1, 2, 3
Article Information
Identifiers and Pagination:
Year: 2014Volume: 10
First Page: 103
Last Page: 115
Publisher ID: CPEMH-10-103
DOI: 10.2174/1745017901410010103
Article History:
Received Date: 3/7/2014Revision Received Date: 17/7/2014
Acceptance Date: 2/8/2014
Electronic publication date: 21 /10/2014
Collection year: 2014

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Global population aging over recent years has been linked to poorer health outcomes and higher healthcare expenditure. Policies focusing on healthy aging are currently being developed but a complete understanding of health determinants is needed to guide these efforts. The built environment and other external factors have been added to the International Classification of Functioning as important determinants of health and disability. Although the relationship between the built environment and health has been widely examined in working age adults, research focusing on elderly people is relatively recent. In this review, we provide a comprehensive synthesis of the evidence on the built environment and health in the elderly.
1. INTRODUCTION
The increase in life expectancy over recent decades has led to considerable population ageing, a global process that especially affects Western countries. A 2-fold increase in population over 60 years is expected from 2006 to 2050, when it is believed that the number of elderly people will exceed the population aged under 14 years worldwide [1]. There is a clear relationship between ageing and morbidity, mortality, disability, perceived quality of life and health expenditures [2-9].
Policies regarding population ageing focus on various health determinants, among which housing and the built environment have become important actors [10-13]. As a health determinant, the built environment is a broad term which encompasses buildings, spaces, and products that are created or modified by people [14]. Several theories have been proposed to explain the link between environment and physical activity, such as travel behavior theory, environmental press theory, social learning theory, ecological theory and behavior setting theory [15]. The ecological model described by Stockols in the context of Healthy Environments is a broad framework which takes into account the physicalenvironment and the psychosocial environment [16]. This model highlights the functional links between the aging person and micro-, meso-, and macrosystem levels of the environment, as well as the unstable equilibrium between environment and individual competence in very old age [17]. However, the built environment is not only related to health through physical activity. It is also connected to health through other aspects: falls, pollution, social interaction, safety, economical and climate issues [18-21]. Moreover, the effect of the built environment on elderly people in particular has to be taken into account, as this population tends to spend more time at home and in the community area compared with other age groups [22].
The relationship between the built environment and health has been widely studied during recent years in the general population, focusing on how the built environment impacts a wide range of issues including obesity, physical activity, general health, birth outcomes, mental illness or morbidity [23-32]. Therefore, The International Classification of Functioning, Disability and Health (ICF) has incorporated environmental factors as determinants of health and disability [33].
Reviews focusing on the built environment and health outcomes have been mainly focused on adult population and there is little information about the effect of the built environment on elderly people, especially in community residents [34]. This is especially relevant as the elderly suffer from high morbidity and disability rates. In addition, most information available is focused on the impact on physical activity, whilst other aspects of physical health, mental health and quality of life need to be addressed. It is important to elucidate this association in general population, excluding special care and nursing home which should be analyzed separately. Moreover, reviews have included outcomes referring to both physical and sociocognitive factors, as well as methodological variations and incompleteness in method reporting, so that it is difficult to assess their results [35].
The aim of this review is to summarize the evidence on the built environment and health in the non-dependant community-residing elderly through a review of the literature published over the last 10 years. This review focuses on four aspects:
1) Built environment & Physical health.
2) Built environment & Mental health.
3) Built environment & Life satisfaction variables
4) Study methodologies used in assessing the built environment.
2. METHODS
A systematic review through computer searches of Pubmed and ISI Web of Science were conducted to identify English language studies. Both sources involve a wide range of databases (PubMed, Web of ScienceTM Core Collection, Current Contents Connect®, Derwent Innovations Index®, MEDLINE) which are complementary to get the most relevant papers on this topic. Since the interest for the built environment has grown exponentially over the last years, the search was limited to the last decade (January 2002- December 2012) and then updated to September 2013. Search terms were grouped into three categories: aging (aging, older people, elderly people), built environment (built environment, housing, capacity of building), and health outcomes (health, wellness, wellbeing, disability, quality of life, comorbidity, functional limitations, disabled persons, mentally disabled persons) (Fig. 1).
 |
Fig. (1). Search strategy summary with keywords. |
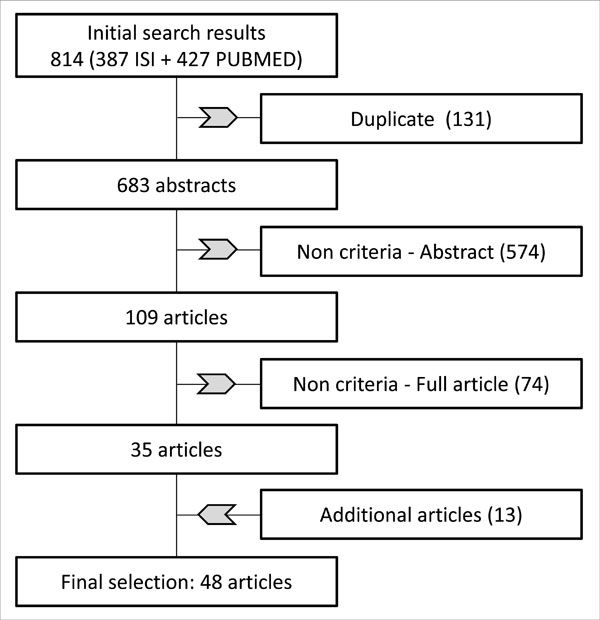 |
Fig. (2). Methodological proceedings and results of the search. |
Search procedures were implemented to obtain the best possible evidence. Duplicates were deleted. Abstracts were selected for further examination where they met criteria and then full article was reviewed to determine whether it was suitable for inclusion. Selection criteria were:
- Age selection criteria: study population groups of individuals over 50 years and studies with specific analysis of people aged over 50 years. Studies with other age selection criteria but reporting on a mean age over 55 years were also included.
- Articles focusing on the effect of economical or psychosocial circumstances (e.g. housing tenure, security, welfare benefits) on health outcomes were excluded.
- Articles including dependent population and elderly people living in institutions or housing for the elderly (e.g. retirement community) were excluded, as people in these situations were considered to live in adapted communities with special care, which would require a specific analysis depending on the patient needs.
Non original articles, qualitative studies and reviews were initially excluded. However, text reviews of these articles were used to identify additional articles. Additional assessment of all the introductions and discussions regarding all the selected original articles was performed to maximize the volume of articles meeting our inclusion criteria. In order to summarize the results of the search, studies were sorted by the following groups: 1) physical health; 2) mental health and 3) a combined group including concepts related with life satisfaction (quality of life, wellbeing, successful ageing, and healthy ageing).
3. RESULTS AND DISCUSSIONS
By using the established criteria, we found 48 articles focusing on the relationship between aging, the built environment and health. The results of the search are summarized in Fig. (2).
The results and discussions of evidence found in the selected studies are categorized under the following major headings: a) physical health; b) mental health; c) life satisfaction.
3.1. Physical Health
Most of the selected studies assessed physical health (n=34), taken as a broad term including preventive care, functioning and disability, injuries and other health-related conditions (e.g. perceived health, hypertension, arthritis symptoms, mortality) (Table 1).
Details of reviewed articles of physical health, preventive healthcare and the built environment.
| Author | Sample (n, country) |
Age | Independent variables (BE) | BE Variable |
Health Variable | Statistical Association |
|---|---|---|---|---|---|---|
| Balfour & Kaplan [47] | 883 USA |
≥55 | 1. Heavy traffic 2. Excessive noise 3. Access to public transportation 4. Inadequate lightning |
S | Risk for loss of physical function | NS + NS + |
| Breeze et al. [49] | 24654 UK |
≥75 | 1. Population density | O | Vaccination | NS |
| Camilloni et al. [36] | 214 Italy |
65-85 | 1. Poor illumination 2. Minor repairs |
S | Home injury risk | + NS |
| Chan et al. [37] | 2712 Canada |
≥65 | 1. Population density 2. Repairs required |
O |
Falls | NS + |
| Clarke et al. [14] | 1195 USA |
≥45 | 1. Neighborhood disorder 2. Any street in fair/poor condition |
O | a. Some disability b. Severe disability a. Some disability b. Severe disability |
NS NS + + |
| Clarke & George [48] | 4154 USA |
≥65 | 1.Housing Density 2. Land-Use Diversity 3. Housing quality variable |
M | Disability | NS (- for ADL in patients with severe lower extremity functional limitations) NS (- for IADL by lower extremity functional limitations) - |
| Clarke et al. [33] | 1225 USA |
≥45 | 1. Poor street condition 2. Heavy traffic 3. Neighborhood 4. Public transit line nearby |
O | Preventive health care use | NS + NS NS |
| Clarke et al. [46] | 1787 USA |
≥45 | 1. Population density 2. Commuting to work by public transit or by walking 3. Age structure |
O | Mobility disability | NS - (only in patients ≥75) NS |
| Dogan et al. [38] | 102 Turkey |
Mean age: 71.4 years | 1. Rooms have good daylight 2. Bathing/showering facilities and accessibility |
S | Home injuries | - - |
| Evci et al. [39] | 3211 Turkey |
>60 | 1. Poor housing conditions | M | Home accidents | + |
| Freedman et al. [45] | 15480 USA |
≥55 | 1. Connectivity 2. Density of population 3. Air pollution |
O | a. Lower Body Limitation b. IADL c. ADL a. Lower Body Limitation b. IADL c. ADL a. Lower Body Limitation b. IADL c. ADL |
NS - (in men) NS NS NS NS NS NS NS |
| Gill et al. [40] | 2619 Australia |
≥65 | 1. Type of dwelling 2. Repair requirement |
S | Falls | NS + |
| Huang [42] | 1212 Taiwan |
≥65 | 1. Location (urban) 2. Housing type (without stairs) |
O | Potential Home environmental hazards | + + |
| Iwarsson et al. [54] | 397 Sweden |
80-89 | 1. Environmental barriers 2. Accessibility problems score 3. Usability in my home-Environmental aspects |
M | Perceived Health | + + + |
| Iwarsson [44] | 72 Sweden |
75-84 | 1. Housing environment | M | ADL-IADL dependence | + (at 6 year follow-up) |
| Lang et al. [50] | 2946 UK |
≥65 | 1. Degree of urbanization | O | Use of dental service | NS |
| Malhotra et al. [55] | 4494 Singapore | ≥60 | 1. Housing type (≤ 2 room) | S | Hypertension | + |
| Mishra [56] | 38595 India |
≥60 | 1. Non clean fuel 2. House type 3. Separate kitchen 4. Urban/rural |
O | Asthma | + + - + |
| Morris et al. [43] | 136 women with multiple sclerosis USA |
NA Mean age: 69.6 years |
1. Density 2. Land use 3. Access 4. Connectivity 5. Walking/cycling 6. Aesthetics 7. Traffic safety 8. Neighborhood satisfaction |
S | Disability | NS NS NS NS + + + + |
| Niemann et al. [57] | NA Europe |
≥60 subgroup | 1. Annoyance by traffic noise | S | a. Cardiovascular risk b. Respiratory c. Neuro-psychic d. Arthritis symptoms |
NS NS NS + |
| Osman et al. [58] | 148 COPD patients UK |
NA Mean: 69 years |
1. Living room over 21ºC 2. Bedroom over 18ºC |
O | a. Respiratory health status b. Health status a. Respiratory health status b. Health status |
NS (+ for symptoms and disease impact) + NS (+ for symptoms) NS |
| Osman et al. [59] | 178 COPD patients UK |
NA Mean >70 years |
1. Home Energy efficiency | O | Respiratory health | + |
| Parra et al. [62] | 1966 Colombia |
≥65 | 1. Street noise 2. Safety from traffic 3. Park density 4. Train stations |
M | Self-rated health | NS + NS NS |
| Pluijm et al. [41] | 1365 Netherland |
≥65 | 1. Highly urbanized area | O | Recurrent falling | + |
| Rudge et al. [60] | 25000 UK |
≥65 | 1. Energy inefficient housing | O | Excess Winter comorbidity | + |
| Singh [61] | 778 India |
≥60 | 1. Type of house [kuchcha vs pucca) 2. Source of drinking water 3. Type of fuel for cooking 4. Type of toilet facility 5. Density of living room |
M | Morbid conditions | + NS NS NS + |
| Takano et al. [51] | 2211 Japan |
NA Mean: 73 years at baseline |
1. Space for taking strolls 2. Parks and tree lined streets 3. Noise from automobiles and factories 4. Garden 5. Regular bus service |
S | Five years survival | + + NS NS NS |
| Vandertorren et al. [53] | 597 heat-related deaths France |
≥65 | 1. Construction date 2. Comfort level 3. Lack of thermal insulation 4. Living on top floor 5. Number of rooms 6. Number of windows 7. Floor 8. Location directly under the roof 9. Duration of sunlight there 10. Temperature 11. Vegetation index |
O | Death risk | + + + + - + NS + + + - |
| Webb et al. [64] | 4763 UK |
≥50 | 1. Housing problems | S | COPD | NS |
| Wen et al. [65] | 229 USA |
≥50 | 1. Perceived physical environment | S | Self-rated health | + |
| Werngren-ElgstrÖm [63] | 31 Sweden (baseline) |
75-84 | 1. Person-environment fit (accessibility) | M | Ill-health symptoms | + |
| Wilson et al. [67] | 5630 US |
≥70 | 1. Type of housing | S | Hip fracture risk | + (mobile home vs house) ; NS (Apartment vs house) |
| Windle et al. [66] | 411 UK |
≥70 | 1. Difficulties scale 2. Cold in bed 3. Cold with current heating 4. Age of the building 5. No roof/loft insulation |
S | Health Status | - NS - NS NS |
| Zuluaga et al. [52] | 433 older patients hospitalized for heart failure Spain |
≥65 | 1. House lacking an elevator 2. House lacking running water 3. House lacking heating 4. No indoor bathroom 5. No bathtub or shower 6. No individual bedroom 7. No automatic washing machine 8. No telephone 9. Feeling frequently cold |
S | Mortality of patients hospitalized for heart failure | + NS NS NS NS NS NS NS + |
(+) Statistically significant, positive effect on outcome; (-) Statistically significant, negative effect on outcome; (NS) Not statistically significant; (O) Objective measure of BE; (S) Self-rated measure of BE; (M) Mixed measure, including objective and self-rate; (NA) Data not available; (COPD) chronic obstructive pulmonary disease; (ADL) activities of daily living; (IADL) instrumental activities of daily living.
Details of reviewed articles of mental conditions and the built environment.
| Author | Sample (n, country) |
Age | Independent Variables (BE) | BE Variable |
Health variable | Statistical Association |
|---|---|---|---|---|---|---|
| Berke et al. [84] | 740 USA |
≥65 | 1. Walkability score | O | Depressive symptoms | - (for men); NS (for women) |
| Brown et al. [86] | 273 low-socioeconomic-status Hispanics USA |
≥65 | 1. Front entrance variables 2. Window area 3. Low sill height 4. Ground-floor parking 5. Small setback |
O | Psychological distress | NS NS NS NS NS |
| Chan et al. [80] | 4489 Singapore | ≥60 | 1. Housing type ≤2 rooms | S | Depressive symptoms | + |
| Evans et al. [85] | 497 USA |
≥60 | 1. Housing quality | O | Positive affect | NS |
| Howden-Chapman [78] | 6762 UK |
55-80 | 1. Housing Quality problems | S | Minor psychiatric morbidity | + |
| Lai & Guo [81] | 497 China |
≥60 | 1. Satisfaction with housing | S | Depressive symptoms | - |
| Saarlos et al. [82] | 5218 men Australia |
65-79 | 1. Walkability 2. Street connectivity 3. Residential density 4. Land-use mix 5. Retail availability |
O | Depression rate | NS NS NS + + |
| Stewart et al. [83] | 218 UK |
≥65 | 1. Accommodation quality | O | Depression | - |
(+) Statistically significant, positive effect on outcome; (-) Statistically significant, negative effect on outcome; (NS) Not statistically significant; (O) Objective measure of BE; (S) Self-rated measure of BE; (M) Mixed measure, including objective and self-rate.
Details of reviewed articles of quality of life, well-being, successful aging and the built environment.
| Author | Sample (n, country) |
Age | Independent Variables (BE Only) |
BE Variable |
Health Variable | Statistical Association |
|---|---|---|---|---|---|---|
| Carta et al. [101] | 399 Italy |
≥65 subgroup | 1. Urbanicity (urban/rural) | O | Quality of life | NS |
| Clarke et al. [33] | 1225 USA |
≥45 | 1. Poor street condition 2. Heavy traffic 3. Public transit line nearby |
O | Interpersonal interaction | NS + NS |
| Iwarsson et al. [54] | 397 Sweden |
80-89 | 1. Environmental barriers 2. Accessibility problems score 3. Usability in my home-Environmental aspects |
M | Life satisfaction | NS - + |
| Ng et al. [98] | 1281 China |
≥65 | 1. Housing type (>3 rooms) |
S | Successful Aging | + |
| Oswald et al. [96] | 1918 Sweden Germany UK Hungary Latvia |
75-89 | 1. Housing variable set 1.a. Environmental barriers 1.b. Magnitude of accessibility problems 2. Housing satisfaction 3. Usability (Physical environmental aspects) |
M | Healthy Aging |
NS - NS + |
| Oswald et al. [100] | 412 Germany |
55-99 | 1. Housing amenities 2. Satisfaction with home environment 3. Satisfaction with outdoor environment 4. Place attachment |
M | General life satisfaction | + (Eastern Region) + (Western Region) + (Eastern Region) NS |
| Oswald et al. [97] | 381 Germany |
>65 | 1. Number of rooms 2. Size in m2 3. Housing accessibility 4. Housing comfort 5. Neighborhood quality 6. Outdoor place attachment |
S | Life Satisfaction | NS - (+ for 65-79 years) NS NS + + |
| Phillips et al. [99] | 518 Hong Kong |
≥60 | 1. Interior environment 2. Exterior environment 3. Residential satisfaction |
S | Psychological wellbeing | + + + |
| Werngren-ElstrÖm et al. [63] | 31 Sweden (only baseline results; follow-ups included sheltered-living) |
75-84 | 1. Person-environment fit (accessibility) | M | Subjective well-being | NS |
| Parra et al. [62] | 1966 Colombia |
≥65 | 1. Street noise 2. Safety from traffic 3. Park density 4. Train stations |
M | a. Physical dimension of QOL b. Mental dimension of QOL a. Physical dimension of QOL b. Mental dimension of QOL a. Physical dimension of QOL b. Mental dimension of QOL a. Physical dimension of QOL b. Mental dimension of QOL |
+ + + + NS NS NS NS |
(+) Statistically significant, positive effect on outcome; (-) Statistically significant, negative effect on outcome; (NS) Not statistically significant; (O) Objective measure of BE; (S) Self-rated measure of BE; (M) Mixed measure, including objective and self-rate.
Seven studies focused on the relationship between the built environment and injuries [36-42]. The approach in these studies was through examination of distinct variables, e.g. falls, home injuries, home hazards and hip-fracture risk. All of the studies linked at least one built environment variable (built environment variable) with this issue. For example, Dogan et al. (2005) found an association between bathing facilities and home injuries [38] . The built environment variables associated with injuries included mainly housing issues. Similar results were observed in the seven articles focusing on disability or functioning [14, 43-48]. In that case, outdoor built environment variables such as connectivity, excessive noise, inadequate lightning or street condition were related to disability [14, 43, 47]. Preventive health was assessed through vaccination, preventive health care and use of dental service in three studies [33, 49, 50]. No evidence supporting a relationship between preventive health care and the built environment was found. The association between built environment and mortality was associated in three studies. For example, one study found that the presence of parks, tree lined streets and space for taking strolls was associated with higher five-year survival [51]. At an indoor level, differences were found in the other two studies, in which variables related to temperature, such as feeling cold or lack of thermal insulation, were associated with mortality [52, 53]. Other associations between physical health and built environment found in the selected studies included self-rate health, comorbidity, arthritis symptoms, hip fracture risk, hypertension and asthma [54-67].
Studies on physical health have some specific limitations. First of all the variety of variables and definitions used, which difficult comparison between studies. Moreover, reduced capacity may affect walking activity and could lead to a different perception of the neighborhood, which may skew the results [62, 68]. Furthermore, there could be a bias caused by the possibility that active elderly people may choose to live in more-walkable neighborhoods [62, 69-71]. In addition to the direct effect on physical functioning, environment may also influence social support and psychological distress, and this can also impact physical functioning. One study found a significant association between the presence of variables that are thought to promote social contacts (more front porches, stoops and buildings built above grade) and physical functioning, but this model requires further investigation [71].
The built environment has been shown to impact on physical health at different levels. It has been previously stated that the built environment can limit or promote the ability to complete specific actions [72]. A better physical functioning may be related to some of the physical health results, especially taking into account the nature of some built environment variables such as walkability and connectivity. Other specific variables would be related to specific domains, e.g. indoor issues and injuries, temperature concerns and mortality [73]. A model including built environment enlarges the medical model that typically focuses on the individual and pathology connecting the person with the environment [74] . Our results support the review by Cunningham & Michael (2004), which concluded that environmental factors should be taken into account rather than concentrating solely on specific efforts to promote physical activity [15]. However, there is need to foster the knowledge of specific environmental variables on health outcomes such as injuries, disability and chronic conditions. In addition, various approaches are needed to assess the indirect role of the built environment in physical health through variables such as social support or psychological distress [71].
3.2. Mental Health
Mental disorders are common in elderly people, reaching 20% prevalence in those without dementia aged 65 years and older [75]. However, most research on the built environment has focused on physical health compared with the research regarding mental health [26, 76, 77]. In the elderly, the immediate urban environment becomes an important issue. People tend to spend more time in this environment because of physical decline, retirement, decreased access to transport and shrinking in social networks. Psychosocial processes related to these features would be connected to mental health in several ways [78, 79].
Only eight studies were found to assess mental health, of which five assessed the influence on depression (Table 2) [80-84]. Depression prevalence was linked to the number of rooms in the house, satisfaction with housing, housing quality, land-use mix and retail availability, whilst no relation was found regarding residential density, street connectivity, and walkability. For example, Lai & Guo (2012) found that satisfaction with housing was associated with fewer depressive symptoms [81]. One study examining psychological distress and another one assessing positive affect did not find any link between the built environment and these variables [85, 86]. Finally, Howden-Chapman et al. (2011) found a direct relationship between housing quality problems (including home size, need of repairs and presence of moisture) and minor psychiatric morbidity measured with the General Health Questionnaire (GHQ-30) [78].
Among these studies, methodological difficulties were found regarding the variability of the assessed variables and the differences in the definitions of mental and environmental variables. For instance, housing quality was assessed in three studies through three different methods [78, 83, 85]. On the other hand, some environmental variables that were previously suggested as mental health mediators, including floor level, noise or indoor air quality, were not assessed in these studies [85]. Another interesting issue to consider in future studies is the possibility that people moving to certain areas may have higher social skills, so that the results can be biased [87]. Furthermore, there might be variables which lack reliability as they were developed specifically for the study and were in some cases confined to a dichotomous answer. Data on confounders such as physical exercise should also be measured in the studies [82, 88, 89].
The effect of the built environment on mental health becomes a delicate issue since it may be difficult to elucidate the effects of physical and social environment [90]. For example, open spaces could lead to social interaction and physical activity which can be linked to individual perceptions, unmet needs and mental health [91]. In fact, it is difficult to separate physical influences from other environmental influences: institutional factors, community factors, policy [92]. However, independent effects on health due to certain environmental factors have been settled in previous studies and further research is needed to promote the more suitable environment for mental health [76].
Most of the evidence found in this review has focused on depression, which has been clearly associated with some environmental variables. Little evidence has been found in other variables such as positive affect, psychological distress and minor psychiatric morbidity. More research is necessary to establish more precise interaction with mental health, especially in conditions others than depression.
3.3. Life Satisfaction and Related Variables
Quality of life (QOL) is a broad multidimensional concept that usually includes subjective evaluations of both positive and negative aspects of life, whilst well-being is defined as a category of phenomena that reflects satisfaction with various domains of life, global judgments of life satisfaction, and current affective state [93, 94]. The WHO has considered the enhancement of quality of life as a major issue in ageing, leading to an increased interest in the relationship with the built environment in recent years [12, 95].
Ten studies focused on quality of life, well-being and related concepts such as life satisfaction or successful aging [33, 54, 62, 63, 96-101] (Table 3). Among these studies, several distinct environment variables were used, so that a broad analysis was not possible. However, it is noticeable that the Housing Enabler was used as the instrument for assessing accessibility in three of the studies [54, 63, 96]. Two of the studies using this instrument found a link between accessibility and both life satisfaction and healthy aging, whilst the study by Werngren-Elgström et al. (2009) did not find a relationship with subjective well-being [63]. Accessibility was also assessed in another study and showed no effect on life satisfaction for most of the built environment variables [97].
Apart from accessibility, other variables were significantly associated with health outcomes. For example, variables such as residential satisfaction, home size, housing type, heavy traffic, higher usability, exterior environment, interior environment, street noise and safety from traffic were associated with quality of life, well-being, life satisfaction or successful aging [33, 54, 62, 96-100]. However, the following variables were not connected with life satisfaction, well-being and quality of life: urbanicity (urban/rural), poor street condition, public transit line nearby, park density, number of train stations, housing comfort, number of rooms, environmental barriers, housing satisfaction and neighborhood quality 33, 54, 62, 96, 97, 101.
As observed in the previous health domains but especially in this case, there is a high degree of variability in methodology and results. The fact that almost every study focused on different environmental variables or similar variables with a different approach makes it difficult to hypothesize on the nature of the relationship. Several models connecting environmental factors and quality of life have emerged in recent years. Sugiyama & Thompson (2007) proposed four different models. One model states that environmental factors may be a proximal predictor of quality of life [91]. In contrast, the other models involve indirect associations through outdoor activity, personal factors, personal projects and unmet needs. All these issues suggest the need for further research into the model so that studies could focus on the factors with the greatest impact on quality of life.
3.4. Methodology in Built Environment Research
Methodological concerns arise in the studies connecting the built environment and health, among which the variety of variables and the lack of constant definitions or measure units are highlighted. According to the type of built environment measure, the articles could be classified as objective (20 papers), self-report (19 papers), mixed studies involving both objective and self-reported measures (9 papers).
Two types of objective measures can be distinguished: a) those derived from geographic measures, census tracts or similar databases and b) those from interviewers acting as observers in streets and homes. Several instruments and tools have emerged in recent years for the objective assessment of environmental issues. These instruments produce a single score linking the built environment and health. The following designed tools were found to assess the impact of the built environment on elderly people:
- Walkability index of the Walkable and Bikable Communities Project (WBC) [84]. This index contains data from Geographic Information System (GIS) and public sources about specific items. Circular buffers of 100, 500, and 1000 meters were created around each point.
- University of Miami Built environment coding system – UMBECS [86]. It assesses 76 features regarding the built environment, although few of them were finally used in the selected studies: front entrance, window area, low sill height, ground-floor parking, and small setback.
- Systematic social observation system [14, 33]. This validated examination is also based on a direct observational method, rating several conditions: curbs, holes, etc.
There are some reservations regarding the use of these instruments. Firstly, the use of a composite variable could fail to take into account individual features that could matter in mental health, physical health or quality of life [82]. Secondly, it may be difficult to compare the results, given that they assess distinct domains of the built environment. Furthermore, there may be interviewer bias, and therefore interviewers should be trained to administer these instruments. Finally, it is important to demonstrate their validity and reliability but only the Systematic Social Observation System and the Walkability index were found to be validated tools, and only for general population [102, 103].
Studies with self-reported built-environment variables represent a similar volume of evidence as the group of studies with objective measures. Subjective evaluation has high individual variability so self-report validation is needed to get more accurate results [36]. Among the 19 articles using a subjective measure of the built environment, only one standardized tool was used: the neighborhood environment walking scale – NEWS [43]. The NEWS survey is a validated tool which involves perceptions of nine environmental characteristics at a neighborhood level [104, 105]. However, elderly-based validation is needed [104-106]. The other reported studies using self-rating measures obtained most of the results from five-item Likert scales and dichotomic scales. Self-perception of housing was considered a non-specific measure in some analyses. This can result in very positive ratings if asking about satisfaction in general terms, so it was considered that reliability would be strengthened by independent measures [54, 78, 97]. Moreover, it is thought that subjective opinions in poorer circumstances could be linked to a negative world view that could lead to more perceived difficulties with regard to housing and severity of illness [66]. Finally, self-report questionnaires for elderly people have to be short and easy to understand, which might hinder the use of some variables due to their complexity [97].
Only 9 studies assessed the built-environment variables through the combination of both objective and self-rated measures, which provides a more comprehensive assessment [43]. This approach aims to reduce the subjectivity of the measurements while keeping the individual perception that could also result in different physical behaviours. In some cases, GIS data might not be representative of the perceived neighborhood. With respect to standardized tools, four studies used the Housing enabler [44, 54, 63, 96]. This tool has been validated but there is still a need for it to be validated in the elderly population [107, 108]. The Housing enabler consists of an initial step to assess functional limitations; combining an interview with direct observation. The second step assesses physical barriers objectively, and then an accessibility score is calculated based on the first two steps [107, 109]. However, these studies selected different variables from the Housing enabler tool for data analysis.
Built-environment related variables may also be classified according to the space on which the study was focused a) indoor variables, defined as immediate domestic home environment and b) outdoor variables or neighborhood variables, defined as the immediate out-of-home environment [97]. Both types of variables may be needed since, as stated before, indoor or outdoor variables may be independently linked to specific domains of health. However, as with other issues connected with the built environment research, there is no clear agreement on definitions and a single framework is needed.
Another methodological issue is the type of design used. The information collected from these studies came mainly from cross-sectional data, making the establishment of a causal link methodologically difficult [80, 97]. Despite data suggesting the effects of the built environment on several health issues, the association cannot be described as beyond doubt, and the few prospective studies have a limited observational period. Only 9 out of the total of 48 papers assessed longitudinal data, among which only four studies had information gathered over five or more years [44, 51, 52, 78]. Furthermore, environments change over time and this situation can also affect the results of cross-sectional data [62]. More longitudinal studies are needed to understand causal and temporal relationships.
Extrapolation of the data to other countries or areas may not be appropriate as many discrepancies regarding housing and urban planning exist between them. Moreover, individual-level information from census and secondary data sets tract often differ from the areas covered on foot compared with a more precise description from individual-level geographical data [45, 46, 84]. There is risk of modifiable areal unit problem (MAUP), scale and aggregation effects resulting in statistical bias[110]. For example, one area scale (e.g, census block) can lead to different results when compared with analysis using another scale (e.g., census tracts). Assuming that participants live in the center of the selected area or changing the shape of the aggregate area can also lead to MAUP [82, 84].
It was considered that some of the studies had insufficient group or subgroup size to make strong statistical inferences [52, 54, 62, 100]. Some studies had a considerable loss of enrolled participants, a high number of people who refused to participate or participation bias, all of which can lead to misinterpretation of the results [36, 78, 101]. It has been suggested that in some studies, cases were more predisposed than controls to report problems. This could happen, for example, when reporting the risks of accidents at home [36]. Another possible source of bias is the fact that some people may be recent arrivals in a neighborhood and their current health could be affected to a greater extent by their previous place of residence. The same could happen with regard to socioeconomic status [49]. It is important to take into account the influence of several intermediate individual factors, such as family support, baseline health status, health policies or social engagement so that the inferences can be made with confidence that the built environment is the single most relevant factor underlying the results in health [42, 45, 84].
On some occasions, long-term dwellers were the target of the study, which could be considered positive as they had been living long enough in the area for a possible interaction between the built environment and health to be established. On the other hand, it could lead to reduced potential to detect the problems in cases where subjective variables were used [47].
3.5. Implications for Health Policy and Future Research
Ideally, people should not need to move to be in a supportive environment, but there is a need for elder-friendly knowledge, including terms of equity [111]. Historically, policy makers have focused their attention on the study of long-term care, social affairs and health care but the impact of built-environment has rarely been investigated explicitly [112]. The evidence that has arisen during recent years has led to interest in and promotion of age-friendly cities but there is need for policy implementation at a national and local levels [112]. As clear associations are found, urban planning innovation should become a major aim for stakeholders considering expected aging predictions.
There is a need to agree on how to proceed with the built-environment assessment, taking a broad approach and unifying theoretical framework to aid understanding [22, 113]. Neighborhoods change over time and an individual may move several times in life [22]. Wiles et al. (2009) conducted a qualitative study that led to the definition of the “social space”, capturing the “elastic physical, imaginative, emotional and symbolic experiences of and connections to people and place across time and in scope” [114]. Moreover, the association between the built environment and personal characteristics may have a dynamic interaction that has not been thoroughly explored [92]. It is important to take into account different levels (housing, neighborhood, transportation since bias could occur as a result of focusing on a specific level [113, 115]. However, in some health domains (e.g. health and thermal insulation) only one level may suitable. Confounding factors (age, education, managing stress, health behaviors, religious coping, financial status, etc), which might be responsible for some of the results, should also be assessed [22, 112].
Our review has limitations. Age selection aimed to select participants over 50 years following a similar approach in other papers and reviews on this topic, but there are reviews which take 60-65 years of age as a reference, which could affect the final interpretation [72, 116]. Separately, the latter stages of the life are linked to declining health, financial deprivation and social isolation [22]. This situation differs among countries and hampers extrapolation. Moreover, there has been a lack of standardized terminology regarding the built environment for years and most studies have adapted their own type of measurements so that similar variables may not imply similar approach, and a different implication for health. Some efforts have been made in recent years to summarize them, such as the Healthy Places Terminology Directory of the CDC and the European Environment Information and Observation Network’s Thesaurus [117, 118]. Articles including populations living in institutions or any housing for the elderly (e.g. retirement community) were excluded as these are special populations living in adapted communities with special care. It would be interesting to assess these groups to detect any possible association that could lead to fostering the best health policies for them. Finally, the purpose of this review was to provide a comprehensive synthesis of the evidence on the built environment and health in the elderly, but in order to identify clear patterns of association meta-analysis would be needed.
CONCLUSION
Although with some methodological limitations, the evidence reviewed in this paper suggests that some built-environment variables may impact on health, especially in some specific issues. There is need for further investigation to clarifying this relationship, and this should be achieved through large samples using longitudinal studies. These should consider different level environment domains through similar frameworks including objective and subjective validated evaluations to enable reliability and comparability within and among them. Furthermore, the identification of clear associations between health and built environment could have a beneficial impact on future public policy making.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The research leading to these results has received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under grant agreement number 223071 (COURAGE in Europe) and the Spanish Ministry of Education, Culture and Sport (FPU12/05661). Additional support was provided by funds from the Instituto de Salud Carlos III-FIS research grants number PS09/00295 and PS09/01845, from the Spanish Ministry of Science and Innovation’s ACI-Promociona (ACI2009-1010) and the Fundació Recercaixa (An age-friendly city for a successful ageing project). This article is part of a PhD programme developed in the Public Health Department of the Universitat de Barcelona, Spain.