All published articles of this journal are available on ScienceDirect.
Defining the Optimal Threshold Score for Panic Agoraphobic Spectrum - Short Version (PAS-SV) Questionnaire in Clinical and General Population
Abstract
Background
The Panic Agoraphobic Spectrum - Short Version (PAS-SV) Questionnaire evaluates a wide range of symptoms belonging to panic disorder and agoraphobia (PAD), including both full-threshold and sub-threshold symptoms. While the PAS-SV has proven useful for quantifying panic-agoraphobic symptoms, it currently lacks a validated diagnostic threshold.
Aim
This study aimed to determine the optimal cut-off score on the PAS-SV for identifying the presence of clinically significant PAD.
Methods
The study included 54 patients diagnosed with Panic Disorder and Agoraphobia (PAD) and 54 healthy controls (HC). Trained psychiatrists conducted clinical diagnoses based on DSM-5 criteria and subsequently assessed participants using the PAS-SV.
Results
The PAD group exhibited significantly higher PAS-SV scores compared to the healthy control group. The most effective cut-off score for distinguishing subjects with PAD was determined to be 16, demonstrating satisfactory levels of specificity and sensitivity.
Conclusion
Our findings suggest that a cut-off score of 16 on the PAS-SV is the most discriminative in identifying individuals with Panic Disorder and Agoraphobia.
1. INTRODUCTION
1.1. Panic Disorder and Agoraphobia
Panic Disorder (PD) is an extremely frequent anxiety disorder, with prevalence rates in the general population of 2.1 and 4.7% [1, 2]. According to the DSM-5-TR, panic disorder is characterized by unexpected and recurrent panic attacks, followed by worry, fear, and behavioral changes [3]. By panic attack, the DSM-5 means a sudden wave of intense fear or intense discomfort that peaks within minutes, and during this time, four (or more) of thirteen symptoms occur, such as palpitation, sweating and trembling [4]. Panic disorder frequently tends to assume a chronic pattern, significantly impacting quality of life and representing a significant healthcare expense. The chronic nature of PD often necessitates long-term management strategies, which can be both resource-intensive and challenging for patients. Effective interventions and timely treatment are crucial in mitigating the long-term impacts on individuals’ daily functioning and overall well-being. These factors suggest the importance of implementing the effectiveness of the prevention, diagnosis and treatment processes [5]. This need appears even more urgent considering the high rate of comorbidity with other mental disorders, concerning 80 percent of individuals with PD, such as major depressive disorder, alcohol and substance use disorder, and other anxiety disorders [6]. These include Agoraphobia (AG), a diagnosis differentiated from panic disorder in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and characterized by fear and anxiety in agoraphobic situations [3]. A diagnosis of AG can be found in 80.9% of individuals with PD, and several studies have concluded that the coexistence of the two disorders results in a worsening of panic disorder in terms of course, prognosis, and response to treatment [7].
1.2. The Spectrum Model
Beyond an overt diagnosis of a mental disorder, numerous studies have shown that even subthreshold psychopathological symptomatology, not reaching the threshold for meeting DSM criteria, is capable of significantly impacting the individual’s quality of life [8-11]. Several studies have shown how even subthreshold psychopathological manifestations are sometimes capable of impairing an individual's functioning, thus meriting early identification [12-20]. Regarding PD and AG (PAD), some authors highlighted that, beyond the DSM criteria, a parade of other panic-agoraphobic symptoms can occur both in individuals diagnosed with PAD and in patients suffering from other mental disorders, such as separation anxiety disorder or mood disorders, without being able to be framed in a proper diagnosis of PD or AG [11, 18, 21, 22]. In order to capture such subthreshold manifestations, a Structured Clinical Interview for the Panic-Agoraphobic Spectrum (SCI-PAS) and the corresponding self-report form (PAS-SR) were developed as part of the Spectrum Project [11]. The long completion time of the questionnaire, corresponding to about 50 minutes, as well as the outdated nature of some items referring to old diagnostic criteria, led to the development of a revised and shortened version of thetool, called the Panic-Agoraphobic - Short Version (PAS-SV) and characterized by. This version showedhigh level of internal consistency and excellent test-retest reliability [22, 23]. However, to date, the PAS-SV lacks a validated threshold to quantitatively establish the presence of PAD as well. The presence of a validated threshold would allow better use of the instrument as a screening tool in clinical and nonclinical settings. Additionally, having a validated threshold can facilitate early intervention by identifying individuals who may not yet meet full diagnostic criteria but are at risk of developing significant symptoms. This proactive approach could potentially reduce the severity of the disorder and improve long-term outcomes.
2. METHODS
2.1. Participants and Procedure
For the aims of this study, we evaluated a convenient sample consecutively recruited between September 2022 and December 2023 at the Psychiatric Clinic of the University of Pisa. The sample was composed of two groups: patients with full-blown PD or AG (PAD) and healthy controls (HC). The first group was recruited amongst adult outpatients with a PAD diagnosis according to DSM-5 criteria who were following a treatment program for PAD. The Structured Clinical Interview for DSM-5, Research Version (SCID-5-RV) [24] was used to confirm the diagnosis of PD and AG, as well as the absence of mental disorders among HC subjects. All subjects were clinically assessed according to DSM-5 criteria. Moreover, all subjects completed the PAS-SV and the PDSS (Panic Disorder Severity Scale). All subjects enrolled in this research received clear information about the study and had the opportunity to ask questions before they provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Azienda Ospedaliero Universitaria Pisana (reference number 23326).
2.2. Measures
Assessment procedures included the SCID-5-RV [23] and the Panic-Agoraphobic - Short Version (PAS-SV) questionnaire. Evaluations were carried out by psychiatrists, who were trained and certified in the use of the study instruments.
The PAS-SV [22] is composed of 78 items, organized into 4 domains. The first domain investigates the presence of symptoms belonging to a panic attack as described in the DSM-5-TR, while the second domain includes the possible atypical manifestations of panic, i.e., not included within the DSM. The third domain regards the possible concerns and behaviors related to the presence of panic, such as sensitivity to medication, sensitivity to reassurance, and separation anxiety. Finally, the fourth domain explores the presence of agoraphobic and claustrophobic symptoms in different circumstances, both included and not included in the DSM description of “Agoraphobia”. “The PAS-SV was administered in a controlled setting to ensure that participants understood the questions and could respond accurately. The questionnaire's design allows for the assessment of both DSM-5 criteria and subthreshold symptoms, which are critical for capturing the full spectrum of panic and agoraphobic symptoms.
The PDSS is an instrument tailored to evaluate the presence and severity of panic disorder and associated symptoms, featuring seven domains: frequency of panic attacks; distress during panic attacks; anticipatory anxiety; agoraphobic fear and avoidance; interoceptive fear and avoidance; impairment of or interference in work functioning; impairment of or interference in social functioning. Scores are organized on a Likert scale ranging from 0 to 4. A score equal to or above 9 is indicative of a possible PD [24, 25].
2.3. Statistical Analyses
Chi-square tests and ANOVA analyses were employed for comparing socio-demographic variables. The Mann–Whitney U test was used to compare PAS-SV scores among the two groups. A Receiver-Operating Characteristics (ROC) curve was utilized to find the threshold value of the PAS-SV total score that best identifies the subjects meeting the DSM-5 criteria for full-blown PAD. According to the definition of accuracy, the ROC analysis was built on the basis of sensitivity and specificity for different cut-offs. We computed Cohen’s Kappa in order to evaluate the concordance between PAS-SV and PDSS in identifying PD subjects vs HC. Statistical analyses were conducted using SPSS version 26.0 [26].
3. RESULTS
We recruited a total of 108 subjects (Females 57.4%, N = 62; Males 42.6%, N = 46; mean age: 40.44±12.67). The sample was distributed in two groups: 54 PAD (PAD group; Females: 64.8%, N = 35; Males: 35.2%, N = 19; mean age: 41.87 ± 13.03) and 54 healthy controls (HC group; Females: 50.0%, N = 27; Males: 50.0%, N = 27; mean age: 39.02 ± 13.03). The two diagnostic groups did not significantly differ from each other in terms of age (p = 0.475; F = 0.513) and sex (p = 0.120, X2 = 2.424) (Table 1). This demographic balance ensures that the observed differences in PAS-SV scores between the PAD and HC groups are attributable to the presence of panic disorder and agoraphobia rather than age or sex-related factors.
Subjects with PAD reported significantly higher scores (p<.01) on PAS-SV than healthy controls (Table 2 and Fig. 1). According to the ROC analysis, the most discriminant cutoff of the PAS-SV total score for identifying PAD subjects was 16, with an AUC value of 0.999 (p < .001), a sensitivity of 0.981, a specificity of 0.981 (Fig. 2) and a Youden Index of 0.963 (Fig. 2). We found an excellent concordance between PAS-SV and PDSS in identifying PAS subjects vs HC, demonstrated by Cohen’s K =.0.936, p<.001. This high level of concordance suggests that the PAS-SV is a reliable tool for screening and assessing PAD, supporting its utility in both clinical and research settings. The results also highlight the effectiveness of the PAS-SV in capturing a range of symptoms relevant to panic disorder and agoraphobia.
4. DISCUSSION
The aim of this study was to define which score of the PAS-SV should be considered as a threshold value when investigating the presence of PAD among adults. According to our results, the PAS-SV showed an excellent ability to discriminate the presence of Panic Disorder and Agoraphobia. The best threshold value for identifying PAD was a score of 16 (which is obtained with a positive endorsement of 16 items of the questionnaire). This value was associated with good levels of specificity (0.981) and sensibility (0.981). The study further corroborates the validity of PAS-SV domains, showing that PAD patients scored significantly higher than the HC group on each
| - | PAD (N= 54) | HC (N=54) | - | - | |
|---|---|---|---|---|---|
| Mean± DS | Mean± DS | F | p | ||
| Age | 41.87 ± 13.03 | 39.02 ± 13.03 | 513 | 0,475 | |
| - | N(%) | N(%) | Chi-Square | p | |
| Sex | F | 35(64.8) | 27(50) | 2.424 | 0,12 |
| M | 19(35.2) | 27(50) | |||
| PAS-SV |
PAD (N= 54) Mean± DS Mean Rank |
HC (N=54) Mean± DS Mean Rank |
p |
|---|---|---|---|
| Panic symptoms | 9.50±2.833 81.31 |
0.91±1.069 27.69 |
<.001 |
| Atypical panic symptoms | 8.5000±3.63811 80.85 |
0.2593±.75698 28.15 |
<.001 |
| Anxious expectation and maladaptive behavior | 13.0370±4.69027 80.59 |
1.0370±1.42700 28.41 |
<.001 |
| Agoraphobia | 8.9630±4.42959 79.20 |
1.2778±1.35168 29.80 |
<.001 |
| Total | 40.0000±10.97854 81.44 |
3.4815±3.26063 27.56 |
<.001 |
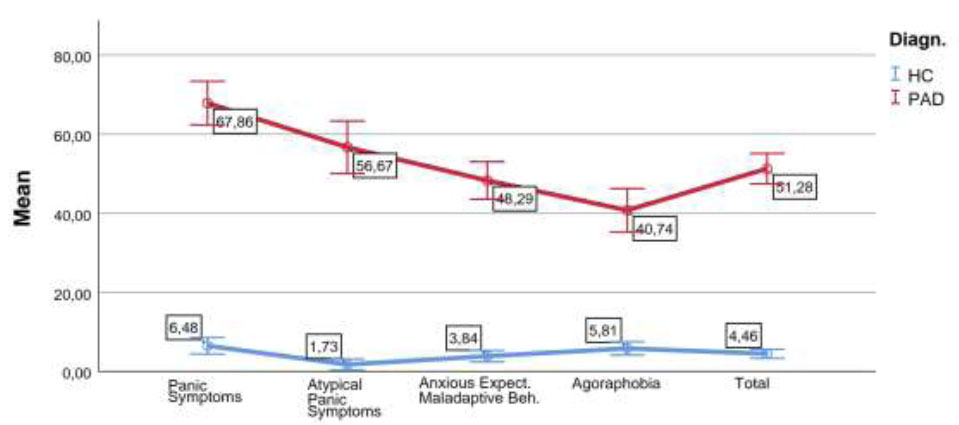
Graphical representation of comparisons between PAS-SV total and domain scores (percentile means) among diagnostic groups (PAD and HC).
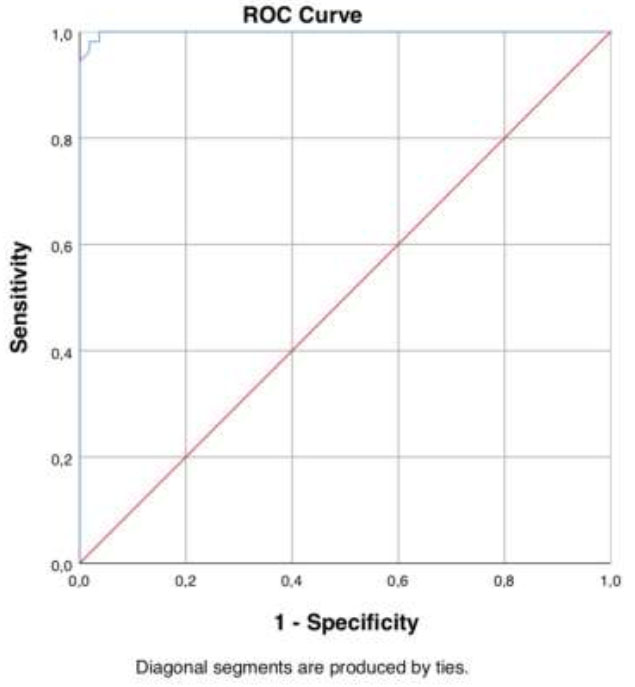
ROC curve of the PAS-SV score for determining PAD. AUC = 0.999; Youden Index =0.963; threshold score = 16.
dimension measured by the PAS-SV questionnaire (“Atypical panic symptoms “; “Anxious expectation and maladaptive behavior”; “Agoraphobia domain”). In clinical settings, the PAS-SV may improve prevention and diagnostic procedures. The ability to screen for PAD early and accurately using the PAS-SV could enhance patient outcomes by facilitating timely intervention and personalized treatment plans. This is particularly important in managing chronic conditions like PAD, where early treatment can significantly alter the course of the disorder. This framework may allow investigation of the presence of PAD - whose role in worsening the psychopathological course and the clinical outcome has been variously stressed in the scientific literature, also in clinical populations of patients with other kinds of mental disorders. However, this work should be considered in light of several limitations. First, our sample was relatively small and a restricted number of demographic characteristics were considered. In addition, the study assesses the presence of a discriminating threshold between the presence and absence of PAD symptoms but not a discriminating threshold between the presence and absence of significant subthreshold panic-agoraphobic traits. This factor limits the use of the questionnaire in assessing subthreshold panic-agoraphobic spectrum symptomatology. Finally, the PAS-SV remains a self-report instrument and therefore susceptible to bias. To address these limitations, future research should consider incorporating additional assessment methods, such as clinician-administered interviews, to provide a more comprehensive evaluation of PAD symptoms and reduce the potential for self-report bias. For these reasons, the PAS-SV should not be used, especially in clinical settings, as the sole diagnostic tool. On the other hand, this questionnaire can be considered, based on these data, as a good screening tool to confirm and further clinical diagnosis among subjects with suspected PAD. Further studies should confirm these findings, eventually in wider samples, from protocols with multicentric, international design, which would allow including a variety of participants from different areas and clinical settings. Moreover, the eventual development of a structured interview-version of PAS-SV will allow overcoming the self-reporting bias in the PAS-SV, although losing the practicality of a self-report tool.
CONCLUSION
The PAS-SV exhibited excellent ability to discriminate the presence of Panic Disorder and Agoraphobia. The best threshold value for the identification of PAD was a score of 16. This value was associated with good levels of specificity (0.981) and sensibility (0.981). Furthermore, patients with panic disorder and agoraphobia scored significantly higher than the HC group on each dimension measured by the PAS-SV questionnaire (“Atypical panic symptoms “; “Anxious expectation and maladaptive behavior”; “Agoraphobia domain”), corroborating the validity of PAS-SV domains.
AUTHOR’S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AG | = Agoraphobia |
| HC | = Healthy Controls |
| PAD | = Panic and Agoraphobia Disorders |
| PAS-SV | = Panic-Agoraphobic Spectrum - Short Version |
| PAS-SR | = Panic-Agoraphobic Spectrum - Self Report |
| PD | = Panic Disorder |
| SCI-PAS | = Structured Clinical Interview for the Panic-Agoraphobic Spectrum |
| SCID-5-RV | = Structured Clinical Interview for DSM-5, Research Version |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the institutional Ethics Committee of Azienda Ospedaliero Universitaria Pisana (reference number 23326).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
ACKNOWLEDGEMENTS
Declared none.


