The School Children Mental Health in Europe (SCMHE) Project: Design and First Results
Abstract
Background : The School Children Mental Health in Europe (SCMHE) project aims to build up a set of indicators to collect and monitor children's mental health in an efficient and comparable methodology across the EU countries. It concerns primary schools children aged 6 to 11 years a range where few data are available whereas school interventions are promising. Methods : Three informants were used: parents, teachers and children. In selecting instruments language, instruments were selected according to the easiness to translate them: SDQ (Strengths and Difficulties Questionnaire) for parents and teachers and DI (Dominic Interactive). A two-step procedure was used: schools randomization then six children by class in each grade. Results : 9084 children from seven countries (Italy, Netherlands, Germany, Romania, Bulgaria, Lithuania, and Turkey) completed the Dominic Interactive in their own language. 6563 teachers and 6031 parents completed their questionnaire, and a total of 5574 interviews have been completed by the 3 informants. The participation rate of the children with parents in the participating schools was about 66.4%. As expected teachers report more externalised problems and less internalised problems than parents. Children report more internalised problems than parents and teachers. Boys have consistently more externalised problems than girls and this is the reverse for internalised problems. Combining the diverse informants and impairment levels children with problems requiring some sort of mental health care were about 9.9%: 76% did not see any mental health professional: 78.7% In Eastern countries 63.1% in Western Europe.
1.. INTRODUCTION
Promoting children and adolescents’ mental health and wellbeing is supported by the literature reviews from the previous chapters. School is there presented as a major setting for interventions. In order to evaluate and monitor these interventions, data collection on child mental health most commune problems is required.
Numerous studies have examined the epidemiology of child and adolescent internalized and externalized disorders in school-age youths [1] (Roberts, Attkisson, & Rosenblatt, 1998). Table 1 presents the results of a meta-analysis of data on the prevalence of internalized and externalized disorders in young people from more than 50 community surveys from around the world, published in the past 15 years (updated from Costello, Mustillo et al., 2004; In IOM; 2009 [2]).
| Diagnosis or Diagnostic Group (N of studies contributing to estimate) |
Prevalence % | Standard Error (%) | Lower 95% | Upper 95% |
|---|---|---|---|---|
| One or more disorders (44) | 17.0 | 1.3 | 14.4 | 19.6 |
| Unipolar depression (31) | 5.2 | 0.7 | 4.0 | 7.0 |
| Any anxiety disorder (29) | 8.0 | 1.0 | 6.2 | 10.3 |
| Generalized anxiety disorder (17) | 1.3 | 0.3 | 0.9 | 2.0 |
| Separation anxiety disorder (17) | 4.1 | 0.9 | 2.6 | 9.4 |
| Social phobia (15) | 4.2 | 1.1 | 2.4 | 7.3 |
| Specific phobia (13) | 3.7 | 1.3 | 1.7 | 7.7 |
| Panic (12) | 0.7 | 0.2 | 0.3 | 1.5 |
| Posttraumatic stress disorder (7) | 0.6 | 0.2 | 0.3 | 1.1 |
| Attention deficit hyperactivity disorder (34) | 4.5 | 0.7 | 3.3 | 6.2 |
| Any disruptive behavior disorder (23) | 6.1 | 0.5 | 5.4 | 7.3 |
| Conduct disorder (28) | 3.5 | 0.5 | 2.7 | 4.7 |
| Oppositional defiant disorder (21) | 2.8 | 0.4 | 2.1 | 3.7 |
| Substance use disorder (12) | 10.3 | 2.2 | 6.3 | 16.2 |
| Alcohol use disorder (9) | 4.3 | 1.4 | 2.1 | 8.9 |
| Countries | Bulgaria | Germany East | Germany West | Italy | Lithuania | The Netherlands |
Romania | Turkey | Total |
|---|---|---|---|---|---|---|---|---|---|
| School participation | |||||||||
| Number of potential schools | 48 | 150 | 150 | 63 | 49 | 48 | 45 | 46 | 599 |
| Number of participating schools | 44 | 12 | 11 | 55 | 42 | 13 | 43 | 38 | 261 |
| % school participation | 91.7% | 8.0% | 7.3% | 87.3% | 85.7% | 27.1% | 95.6% | 82.6% | 43.6% |
| Children participation | |||||||||
| Number of children in participating schools | 2160 | 825 | 826 | 2750 | 2208 | 1660 | 2064 | 1824 | 14317 |
| Children | 1385 | 441 | 445 | 1721 | 1275 | 1503 | 1393 | 921 | 9084 |
| % of children participation | 64.12% | 53.45% | 53.87% | 62.58% | 57.74% | 90.54% | 67.49% | 50.49% | 63.45% |
| Informant participation | |||||||||
| Parents | 1081 | 240 | 238 | 757 | 1159 | 684 | 1206 | 666 | 6031 |
| Teachers | 1267 | 373 | 362 | 1323 | 1226 | 1292 | 1171 | 872 | 7886 |
| 3 informants | 996 | 203 | 194 | 757 | 1118 | 558 | 1106 | 642 | 5574 |
| % of participating children with parent | 78.05% | 54.42% | 53.48% | 43.99% | 90.90% | 45.51% | 86.58% | 72.31% | 66.39% |
| General Practitioner | Pediatrician/ child specialist |
No mental health consultation |
No health consultation at all |
||
|---|---|---|---|---|---|
| N | % | % | % | % | |
| Italy | 44 | 15.9 | 72.7 | 59.1*** | 4.5 |
| Netherlands | 47 | 63.8 * | 29.8 | 57.4*** | 12.8** |
| West Germany | 20 | 85** | 60 | 85.0 | 10.0 |
| West Europe | 111 | 48.6*** | 52.2 | 63.1*** | 9.0 * |
| Bulgaria | 89 | 70.7 | 43.8 | 91.0 * | 4.5 |
| East Germany | 21 | 33.3 | 66.7 | 85.7 | 9.5 |
| Lithuania | 160 | 75 | 25.6 | 75.6*** | 7.5 |
| Romania | 101 | 85.1 | 38.6 | 71.3*** | 7.9 |
| East Europe | 371 | 74.4 | 35.8 | 78.7*** | 7.0 |
| Turkey | 63 | 22.2 | 42.9 | 82.5 | 15.9 |
| TOTAL | 545 | 63.1 * | 40 | 76.0*** | 8.4 * |
In this meta analysis sample size, number of prior months that subjects were asked about in reporting their symptoms and age of participants were controlled. It was observed a mean estimate for any diagnosis of 17% (standard error, SE, 1.3%). Anxiety disorders were common (8%), followed by depressive disorders (5.2 %) and ADHD (4.5%). However, this recent comprehensive review indicated that only a small proportion of these youth actually have sufficiently severe distress or impairment to warrant intervention. Moreover, the prevalence divergences, in part due to different ways to include impairment into the diagnoses, was pointed out as a major obstacle.
Several studies have noted that boys are more likely to present behavioral and externalized disorders while girls have emotional problems (Breton et al., 1999; Fergusson et al., 1993; Goodman et al., 1998; Meltzer et al., 2003; Simonoff et al., 1997) [3-7]. Boys are more likely vulnerable to disorders with early onset, such as disruptive behavior disorders, and ADHD (Rutter, Caspi, and Moffit, 2003) [8]. Otherwise, after puberty, Depression and anxiety increase markedly in girls but not in boys (Rutter, Caspi, and Moffitt, 2003) [8].
Most of children with externalized disorders are likely to suffer from a later internalized disorders, such as anxiety or depressive disorders (Loeber et al., 2000; Messer et al., 2006) [9, 10]. Impact on children daily life is one of the recent issues on children mental health epidemiology and prevention. About half of the children with a diagnosis have a disorder that causes significant functional impairment in their relationships, cognitive, social, or emotional development (Angold, Erkanli et al., 2002; Costello, Egger and Angold, 2005) [11, 12].
Income level, family structure, number of siblings, economic activity and social class are the most current risk factors. Conduct disorders have strongest association with socioeconomic and family characteristics (Ford, Goodman and Meltzer, 2004) [13]. Poverty, adverse life events, low social, economic status and ethnicity have been largely associated with an increased prevalence of childhood psychiatric disorders (Costello et al., 1996; Goodman et al., 1998; Rutter et al., 1976) [5, 14, 15]. Disadvantaged families and urban environments have been linked with behavioral problems in both childhood and early adolescence (Costello et al., 1996; Fombonne, 1994; Rutter et al., 1976) [14-16].
Maternal smoking during pregnancy is a predictor of internalizing as well as externalizing psychopathology in offspring (Ashford et al., 2008; Batstra et al. 2003; Fergusson et al. 1993; Wakschlag et al., 2002, 2006; Wasserman et al., 2001; Weissman et al., 1999; Williams et al., 1998) [17-24]. The association between prenatal smoking and internalizing and externalizing problems persists throughout childhood and late adolescence.
Children of parents with alcohol problems are at greater risk for emotional and behavioral problems (Chen & Weitzman, 2005; DeLucia, Belz, & Chassin, 2001; Edwards, Leonard, & Eiden, 2001) [25-27]. The link between the parental alcohol consumption and the presence of emotional or behavioral problems in childhood have been explained with the lack of positive parenting attitudes and to poor parental control of their child, destructive marital conflict and parenting problems (e.g., Keller et al., 2011) [28].
Indeed negative parenting attitudes may have an impact on children's mental health (Johnson et al., 2001) [29]. Permissive parenting style of mentally ill mothers was linked with higher symptoms of adolescent depression and anxiety related to children who received positive and directive parenting style (Oyserman, Bybee and Mowbray, 2002) [30]. Children with mental disorders were more likely to be frequently punished than those with no mental disorders. In the UK survey (Meltzer et al. 2003) [6], results from parents' questionnaire showed that children with mental health were more frequently shouted at (42%), sent to their room (18%) and grounded (17%) than children without mental health problems.
Studies, which investigated the mental health service use since the 1980s and in the past decade, clearly noticed that most children who need care are not getting it [31], Horwitz et al., 1992 and 1998; Horwitz, Gary, Briggs-Gowan, & Carter, 2003.) [32-34]. Only 10–15% of young people with mental health problems receive help from existing mental health services (WHO 2005) [35]. The reasons of low rates of mental health service use in childhood and adolescence may include unavailability of services, financial obstacles, parents' lack of awareness, motivation or mental health problem recognition, family history of mental illness, lack of appropriate referral pathways, and use of alternative kinds of help. Moreover, the low proportion of children and adolescents who asked professional help could be explained by the difficulty to parents to recognize the presence of mental health problems in the child’s behaviour. The presence of additional physical health and school related problems increased the rate of help-seeking for child psychopathology (Zwaanswijk et al., 2003) [36]. This increase was not the results of better parental problems recognition but only due to the importance of teacher in the detection of the children with mental health problems.
Most of the above references are issued from US, Canada and UK because large epidemiological surveys on school children population are relatively rare in most of the EU state members and hard to compare because, for the few existing, instruments and sampling designs are very different. Indeed obstacles to conduct school surveys in a comparable way are many; among them the very large number of languages in the EU, the cost of conducting large surveys and the difficulties to obtain administrative authorisations to involve schools, to mention the few. These obstacles have to be overcome since results from the countries where surveys are available could not be applied to the diversity of the EU member states plus, as we will see in this chapter, inter member state comparisons are very informative because it allows to compare the impact of different policies in the diverse MS on children mental health and well being.
The School Children Mental Health in Europe (SCMHE) project has been financed by the EU (Grant number 2006336) in order to build up a set of indicators to collect and monitor children's mental health and its major risk factors in an efficient and comparable methodology across the EU countries. In order to evaluate the feasibility of the proposal, large school surveys were experimented in seven European countries. Primary school children population : 6 to 11 year old children were targeted because few data are available for this age range when school interventions seem easier to implement before the symptoms become long lasting and have produced their deleterious effects on school adaptation.
This chapter will report the proposal: the instruments that have been selected in order to measure the children mental health and the most pertinent risk factors, the sampling design and provides some comparative data on prevalence and access to care. In addition it will illustrate the applications by reporting the outlines of some published papers, which combine data on diverse MS policies or global indicators and children mental health as measured by the surveys.
2.. INSTRUMENTS SELECTION
Seven instruments were pre-selected as the most used structured and semi-structured interviews in the literature for the target population: the Dominic Interactive (DI; Valla, Bergeron & Smolla, 2000) [37], the Child and Adolescent Psychiatric Assessment (CAPA; Angold et al., 1995; Angold and Costello, 2000 Not Found, chaged with:Angold & Costello 1995) [38, 39], the Development and Well-Being Assessment (DAWBA; Goodman, Ford, Richards, Gatward, & Meltzer, 2000a) [40], the Strength and Difficulties Questionnaire (SDQ; Goodman, 1997) [41], the Diagnostic Interview Schedule for Children (DISC; Shaffer et al., 1996) [42], the Diagnostic Interview for Children and Adolescents (DICA; Reich, 2000;) and Child Behaviour CheckList (CBCL; Achenbach, 1981; Achenbach and Rescorla, 2001) [43, 44].
All instruments except one (DI) relies on informants usually parents or teachers for children below 11 year. Discrepancies between informants were expected and recommendations were to collect data from the three informants: children, parents and teachers whenever possible. We decided that MH data will be collected from the three informants in a self administrative manner so we have to produce a parent questionnaire and a teacher questionnaire which completed the DI which was proposed trough a computer. Parents and teachers questionnaires were in a pencil paper mode but in one country this was offered on a computerized manner trough a dedicated website.
Language availability was a major concern for this project because so many languages are spoken in the EU. When translation was not available, instruments were selected according to the easiness to translate them. According these criteria SDQ which exists1 in most of the languages required for parents and teachers and DI2 which is supported by pictures integrated into a computer program with few short sentences to be translated have been selected as a kit that could be developed for any EU country desiring to implement such survey.
The translation process was concerning SDQ and DI for the countries where this was not available such as Italy, Romania, Bulgaria, Lithuania and Turkey for both or one of them. Translation was done by experts with back translation with the collaboration of SDQ and DI authors which allows them to integrate these translations into their official web site.
Papers on DI and SDQ translation validation are either submitted or being written. Moreover an external validation process was set up on 578 children from the seven countries in child psychiatric clinics and few no cases using the DAWBA which combines informant report and clinical rating.
DI is a self-administered questionnaire for children aged to 6 to 11 years old. It's a computerized program which proposed to the children to follow a character, usually named Dominic, represented in the cartoon depicts the gender of the child assessed in different situations. Questions are asked in order to ask if the children feel the same than Dominic. 91 precise situations represent symptoms for 7 common DSM-IV childhood psychopathologies (Attention Deficit/Hyperactivity Disorder (ADHD), Conduct Disorder, Oppositional Defiant, Phobias, Separation Anxiety Disorder, Generalized Anxiety Disorder and Major Depressive Disorder) placed in various daily life situations: at home, at school and with other children. The pictures, texts and voices illustrate the abstract emotional and behavioral content of most frequent mental health problems based on DSM-IV symptomatology.
Because the Dominic Interactive is self-administered and computerized, only one research assistant is needed for 5 to 6 interviews. The DI is easy to use: Children, after a short tutorial, respond by using the mouse to click on "Yes" or "No" boxes, thus disclosing their own reactions when they are faced with these situations Cf. Fig. (1). The child's choices are recorded and analyzed automatically by the computer afterward.
Example of DI’s questions: “Do thunderstorms make you feel scared?”
Sampling procedure for a country with 4 grades school.
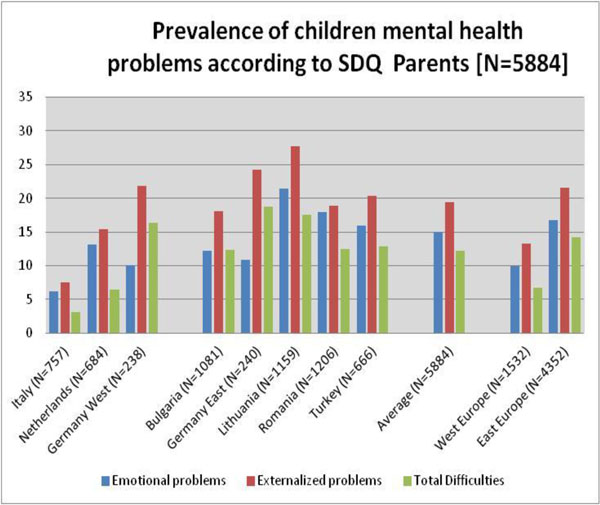
Prevalence of Children probable cases according SDQ Parents (n=5884).
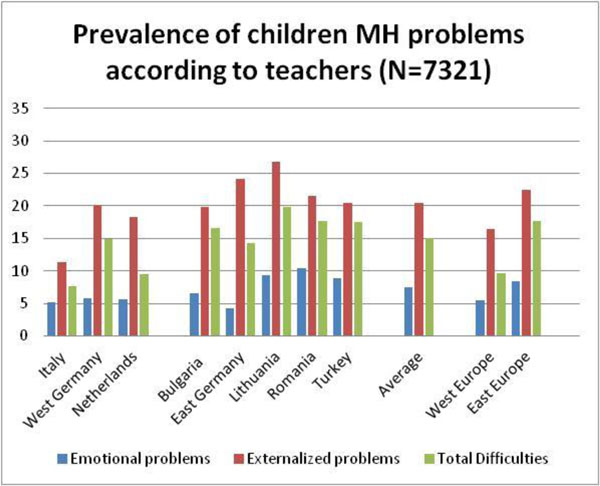
Prevalence of Children probable cases according to SDQ Teachers (n=7320).
Prevalence of Children probable cases according DI (children self reported) n=8327.
At the end, an algorithm assigns the child to one of the three diagnostic probability categories: “likely absent,” “possible” and “likely present” using cut off points reported by Valla et al. (2000) [37]. The DI proposes probabilities to have an Internalized or Externalized diagnosis. For each 7 diagnosis a score is calculated from the different questions/cartoons situations proposed to the child. In Europe it has been validated in France (Shojae 2009) [45].
SDQ, a 25-items behavioural screening questionnaire for children 4-16 years old. (SDQ; Goodman, 1997) [41], predicts probability for psychiatric disorders in child trough an algorithm proposed by its author Robert Goodman (Goodman et al. 2000) [40]. SDQ is constituted of 5 subscales which describe positive and negative attributes of children: 1) emotional symptoms (5 items), 2) conduct problems (5 items), 3) hyperactivity-inattention problems (5 items), 4) peer relationship problem (5 items) and 5) one positive dimension: prosocial behaviour (5 items). “Total difficulties” subscale is the sum of the four first disorders listed above (Emotional symptoms, conduct, Hyperactivity-inattention and peer-relationship problems). “Impact” dimension was calculated from 5 questions for parent, such as Distress question “do the difficulties upset or distress your child?”, impact on home, on friendships, classroom and leisure items. Supplements questions are proposed in order to measure the impact of these difficulties on children and their environment such as problem severity, distress to the child, and interference in everyday life and burden to others. This provides useful additional information for clinicians and researchers with an interest in psychiatric caseness and the determinants of service use (Goodman, 1999) [46].
SDQ has been largely used in diverse surveys in the EU noteworthy in UK (Melzer 2003) not found Goodman et al. 2003) [47], Germany (Woerner 2004) [48], the Netherlands (Van Widenfelt BM 2003) [49] Nordic countries (Smedje H 1999, Obel 2004, Malmberg 2003, Koskelainen M 2000) [50-53], France (Shojae 2009) [45] and in Southern Europe (Marzocchi 2004) [54].
Most of the socio demographic risk factors were collected by the parent questionnaire such as family composition, parent’s age, education and employment statute, country of origin plus question on tobacco consumption including during pregnancy and alcohol behaviour by a 10-item Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993) [55], developed by the World Health Organization (WHO).
In addition the Parenting Scale (Arnold et al., 1993) [56], a 30-item self-report scale covering 3 dysfunctional discipline styles: laxness, over-reactivity and verbosity was added. Parents have to indicate their tendencies to use specific discipline strategies using 7-point Likert scales, where 7 indicates a high probability of making the discipline mistake and 1 indicates a high probability of using an effective, alternative discipline strategy. The total score is the average of all items responses. For calculating scores regarding the 3 different dysfunctionning discipline styles, the average score of the responses on the items on that factor was calculated. Two dimensions were added to the parenting attitudes: autonomy and care, from the Parent Behaviors and Attitudes Questionnaire (PBAQ; Bergeron et al., 1992) [57]. In Italy, 3 dimensions (including punitive behavior) were used since the Parenting scale was not asked. The Care score was the average of 8 items (CF. questions at E2) and 7 items for the Autonomy score (Cf. questions at E3). Parenting attitudes (PBAQ) were classified in 3 categories for each factor: Weak, normal and strong attitude. In addition, a question about the presence of difficulties in the parent and child relationship was asked.
Regarding the parents' mental health measure as a main risk factor, 3 SF-36-subscales were used (Ware and Sherbourne, 1992) [58]. This instrument evaluates negative mental health: the psychological distress and impairment attributable to MH and positive mental health (vitality). It has been widely studied and validated in many languages (International Quality Of Life Assessment [IQOLA]; Ware and Gandek, 1998) [59]. The SF-36 has good construct validity, high internal consistency and high test–retest reliability (Ware et al., 1993, 1994) [60, 61].
In addition some children’s physical health data were asked to the parents: child’s weight and height, presence of asthma/wheezing, eczema and rhinitis, domestic injuries, children life style (exercise, tv and video games time spent) and child’s use of care for mental health problems toward diverse providers.
A self administered questionnaire was provided to the teachers containing SDQ and diverse school competencies levels.
3.. SAMPLE AND PROCEDURES
3.1. Sampling
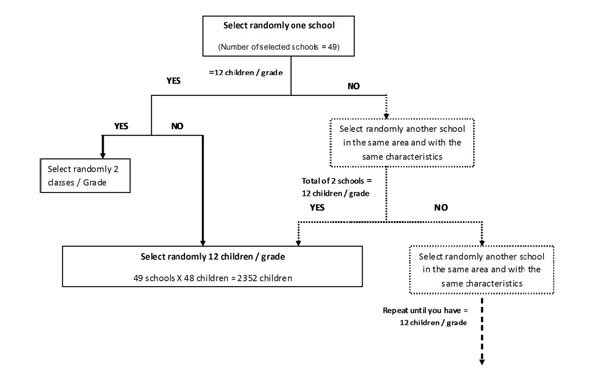
Potential participants were selected from primary schools in each countries. Primary schools were randomly selected in each participating country, classes were randomly selected in each school and 5 to 6 children were randomly selected in each class. In general, 48 children were randomly selected in each school, from 10 for Primary schools with 5 grades to 12 for Primary schools with 4 grades. A total of 45 to 49 schools were needed to obtain about 2500 possible interviews. The Fig. (2) explains the different step for selecting randomly children in each school. Schools were randomly selected, and then we checked if there had more than 12 children by grade. If a school had more than 12 children by grade, only12 children were randomly selected; on the contrary (less than 12), another school was selected in the same area and characteristics in order to complete the correct number of children by schools.
Noteworthy in Germany and in the Netherlands it was very hard to find schools accepting to participate due to many researches going on, so the number of children randomly selected at schools was higher than the other countries.
3.2. Ethical Committee and Authorizations
All the country partners received authorization and support from their government trough their Ministry of Education or Health. Some of the countries only need the authorization from the Ministry of Education (Romania, Bulgaria, and Turkey) for the remaining an ethical approval from the corresponding authority was required and obtained.
Each partner provides a list of schools for the selected areas and then randomly selected schools. The partners were in charge to contact schools. In some countries (Bulgaria and Romania) the Ministry of Education directly sent an information letter with all the contact information in order to participate. Implication of the concerned authority was one of essential step to get schools involved. But for most of the other countries, the teams sent information letter, with the authorization from the ministry, directly to schools and then contact them by phone. At school, the contact was usually the director or vice director. They were in charge to give the list of children, or to select the children randomly and then to give the information and the consent letter to the parents by the children bias.
Parents received the information letter with the consent letter to be sent back to the school with their response; if the parents did not send back the letter of consent with the refusal, the questionnaire was proposed to the three informants. Teachers were allowed to refuse to participate as well; however once the school accepted the survey, teachers were usually positively involved.
The process was identical in each of the countries except in Italy where children were given the DI individually; the six randomly selected children from a class (or less if some parents have sent a refusal) were called and sited in a special room where six computers were waiting for them with ear devices; adequate language, gender was selected by the research attendant who enter their age and a ID number and the child starts the DI. Then he received his parent questionnaire that has to be remit trough the school transmission book where the ID number was written as it was for the teacher questionnaire that was given by the research assistant to the class teacher for the six selected students. At the end of the day, the research assistant leaves with the computers filled with the DI, and with the teacher questionnaires. A secure box was installed at the school where the parents will give back their questionnaires once filled that will be either sent directly to the place where data were entered or collected by the research assistant.
4.. RESULTS
9084 children from seven countries (Italy, Netherlands, Germany, Romania, Bulgaria, Lithuania, and Turkey) completed the Dominic Interactive in their own language. 6563 teachers and 6031 parents completed their questionnaire, and a total of 5574 interviews have been completed by the 3 informants. The participation rate of the children with parents in the participating schools was about 66.4%. see Table 2.
4.1. Main Children Mental Health Results
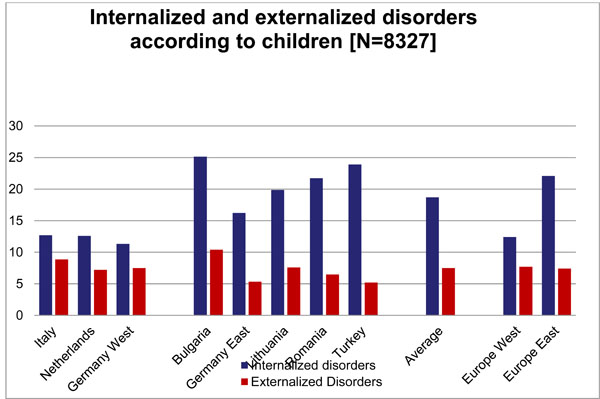
Figs. (3, 4 and 5) present the results for externalised and internalised problems in the different countries by informants: parents, teachers and children.
Problems are more frequent in the West that in the East; Teachers report more externalised problems and less internalised problems than parents. Children report more internalised problems than parents and teachers. Boys have consistently more externalised problems than girls and this is the reverse for internalised problems.
4.2. Access to Care for Mental Health Probles
Responses from the three different informants regarding the child’s mental health problems were combined with the SDQ impact variable in order to produce 4 degrees of mental health care: Children with mental health problems requiring psychiatric care was identified by at least two informants and presented impact. Children with problems requiring non-psychiatric care but still some mental health needs within the primary health care system was identified by at least two informants with or without impact. Problems requiring mental health care grouped the problems requiring psychiatric care and problems not requiring psychiatric care. The two last categories were: children not requiring mental health care were identified by only one informant with or without impact and finally, children without any mental health problems.
According to the above definitions on average 4.4%: have mental health problems requiring psychiatric care. The highest percentage was found in Lithuania (5.7%) and Germany (5.1%) and lowest In Italy (3.2%). Among those children 69.8% were not in contact with any mental health professional; this percentage was ranged from 50% in Italy to 91.1% in Bulgaria. However, 64.3% were in contact with general practitioner: from 18.2% in Turkey to 89.7% in Romania. 42.8% were in contact with a paediatrician: from 26.2% in Lithuania to 78.3% in Italy. Less than 20% among children with psychiatric needs were in contact with a psychologist, psychoanalyst or psychotherapist and or psychiatrist. Bulgaria had the lowest rate with 4.4% for psychiatrist and the lowest rate for psychologist was found in Germany with 5.6%. Italy had the highest rate for psychiatrist (39.1%) and Romania had the highest for psychologist with 50%.
5.1% of the children had mental health problems requiring non-psychiatric care but need mental health care within the primary health care system. Lithuania had the highest rate (8%) and the lowest rate was found in Italy (2.3%). Among those children 76.4% were not in contact with any mental health professional; this percentage was ranged from 59.5% in Romania and 92.7% in Bulgaria. As for children with psychiatric needs, most of the children were mainly in contact with a general practitioner (64.6%) with a highest
rate for Romania (90.4%) and the lowest for Italy (12.5%). Paediatrician was also the second professional the most consulted with 42.5%, and Germany had the highest rate with 70% and the Netherlands the lowest with 20%. Among children with non-psychiatric care but requiring any mental health care from primary care system, 16.2% were cared by psychologist, psychoanalyst and psychotherapist and 11.4% by a psychiatrist or child psychiatrist. In Germany, no children went to see a psychiatrist, but 25% were in contact with psychologist and else. In Bulgaria, the psychiatrist was the less contacted with 2.4% and 7.3% for the psychologist and else. The highest percentage of children seen by a psychiatrist for these problems was found in Italy (25%) and for psychologist and else the highest was found in Romania (34.2%).
Pooling these categories together, children with problems requiring some sort of mental health care were about 9.9%: Lithuania 14,4%, Germany 10.3% and Romania, Turkey and Bulgaria about 9%, and Italy had the lowest rate with 5.8%. 63.1% of these children were cared by general practitioner. 40% were cared by paediatrician or the child specialist. 16.9% of children with problems requiring any mental health care consulted a psychologist, psychoanalyst or psychotherapist was the third the most consulted and the psychiatrist or child psychiatrist went at the fourth place (with 13%). Moreover 76% did not see any mental health professional. In Eastern countries, 78.7% of these children did not see any mental health consultation in Turkey the percentage was nearly 82.5% and in Bulgaria 91%; the situation is a bit better in Western Europe but concern 63.1% of the children Table 3.
4.3. Other Results
40% of the mothers were actually smoking; however important countries differences were found: Bulgaria, Romania and Netherlands were above average whereas Germany, Lithuania and Turkey were below. In addition, attitudes toward smoking in front of children very much differed across countries. Mother’s smoking in the vicinity of children was much lower in Germany, Netherlands and Lithuania than in the other countries. Moreover fathers/companions smoked more often in the vicinity of the children than mother did with a substantial difference in the western regions, with 32% in Bulgaria, 26.5% in Romania, 24% in Turkey and 22.1% in Lithuania versus 5.1% in Germany and 10.5% in the Netherlands.
Mothers did not report excess of alcohol consumption and only a few talked about hazardous drinking and particularly in Lithuania where the percentage was above the average (6.4% versus 2.2%). As an average only 10% of the fathers were respondents but Lithuanian fathers’ rate which was above 20% opposite to the Lithuanian mothers’ rate. As expected, percentages of hazardous drinkers were much higher for fathers/companions than for mothers except in Turkey where both parents reported very low rates.
Mothers’ attitudes towards their children across countries was not particularly more lax, overreactive or aggressive. For laxness, overreactivity and verbosity, less than 20% of the mothers had strong behaviour. However, one-fifth to one-fourth of the Lithuanian, German, Dutch and Romanian mothers esteemed that they had strong or weak caring behaviour, opposite to less than 15% for the Italian and Turkish mothers. Mothers esteemed that they normally promoted autonomy to their child.
4.4. Published Results Concerning Policies and Specific Topics
Beside the few results presented here the data bank comprises huge amount of data from countries where economic indicators and policies largely differ. This allows to compare some behaviours controlling for some expected predictors, according to these policies or country ecological indicators.
To mention the few that have be published thanks to this data bank it was possible to study
- the different tobacco banning policies and parental attitudes toward smoking in the vicinity of their children with a positive effect (Kovess 2013) [62].
- the policies banning physical punishment and the parental declaration of spanking their children in case of misbehaviour and to find a negative correlation after controlling for most of the social expected predictors (Durivage 2014) [63].
- the positive correlation of the rate of car accidents and the children fear of their parents being victims of a car accident (Sowa 2014) [64].
- nutrition policies and children overweight which show large variation across the countries (Olaya 2014) [65].
Due to the large and diverse samples papers have been written on relationship of each parent tobacco smoking during pregnancy and children ADHD which allows to compare father and mother effect and rule out some hypotheses (Kovess 2014) [66], domestic accidents and parental attitudes and mental health correlated (Keyes 2014) [67], child suicidal thoughts and mental health disorders (Kovess 2014) and the list will continue [68].
CONCLUSION
This study has proven that measuring young children mental health was feasible and has showed the adaptability of the selected instruments. This suggests its wider applicability to epidemiologic studies in the diverse EU countries. Substantial information was collected regarding family characteristics, parental attitudes, life-style, and their relationship with mental health problems as well mental health needs completed and not completed in a comparable way that could be linked with health systems in the diverse countries.
This survey also increased people awareness of children mental health problems and their consequences on scholastic competences and problems with access to care and underlined the important role of general practitioners and paediatricians.
The first outcome is the development of a toolkit of three brief and easy to administer instruments for surveying primary school mental health, validated against a diagnosis instrument associated completed by clinician's agreement, which is essential for the credibility of the survey results, internationally as well as nationally.
The second outcome is the results of such surveys using those selected instruments in a comparable manner in the seven participating countries, which underlines
- the high prevalence of mental health problems in EU young children population
- the fact that former Eastern European countries have higher rates than Western but after controlling for social determinants the differences are not longer present although inter countries differences persist
- that parental attitudes also differ between global regions and countries and after controlling for social factors remain different across countries
- that access to care for mental health problems for children is low every where in Europe but lower in the East where re-education is still preferred to psychological care compared to the west
Since young children mental health disorders has been linked to further social job positions and securities (Stanfeld S 2008) [69] this study underlines the need to take care of these children at an age a lot of thinks could be done globally on parents trough positive parental attitudes promotion and at the school and individual level on the attention and provision of adequate care.
In addition the project is providing the first ever data on mental health disorders in some countries where this has never been done (Eastern countries and Turkey) plus it provides data from the children perspective and parental attitudes in all participating countries. It is providing mental health data on specific child populations never studied such as the Rom children living in Romania and Bulgaria compared to that one of the no rom children same age (Lee 2014) [70] or children from non native families in Lithuania.
Finally the project brings attention to an age group which is not well studied: the 6 to 11 age range, where many actions could be done before adolescence, a much more difficult period to set up preventive actions
It brought up many data on parental attitudes and their relationship with children mental health and could support parenting interventions
It will also bring attention to the low access to mental health care resources for those kids and sensitise the school systems
It improves knowledge base on mental health by collecting epidemiological data in a specific age group for which data are scares and interventions very promising.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.
1 www.sdq.org
2 www.dominic interactive.com


