All published articles of this journal are available on ScienceDirect.
PTSD Symptoms Mediate the Effect of Attachment on Pain and Somatisation after Whiplash Injury
Abstract
Introduction:
The development of persistent pain post-whiplash injury is still an unresolved mystery despite the fact that approximately 50% of individuals reporting whiplash develop persistent pain. There is agreement that high initial pain and PTSD symptoms are indicators of a poor prognosis after whiplash injury. Recently attachment insecurity has been proposed as a vulnerability factor for both pain and PTSD. In order to guide treatment it is important to examine possible mechanisms which may cause persistent pain and medically unexplained symptoms after a whiplash injury.
Aim:
The present study examines attachment insecurity and PTSD symptoms as possible vulnerability factors in relation to high levels of pain and somatisation after sub-acute whiplash injury.
Methods:
Data were collected from 327 patients (women = 204) referred consecutively to the emergency unit after acute whiplash injury. Within 1-month post injury, patients answered a questionnaire regarding attachment insecurity, pain, somatisation, and PTSD symptoms. Multiple mediation analyses were performed to assess whether the PTSD symptom clusters mediated the association between attachment insecurity, pain, and somatisation.
Results:
A total of 15% fulfilled the DSM-IV symptom cluster criteria for a possible PTSD diagnosis and 11.6% fulfilled the criteria for somatisation. PTSD increased the likelihood of belonging to the moderate-severe pain group three-fold. In relation to somatisation the likelihood of belonging to the group was almost increased four-fold. The PTSD symptom clusters of avoidance and hyperarousal mediated the association between the attachment dimensions, pain, and somatisation.
Conclusion:
Acknowledging that PTSD is part of the aetiology involved in explaining persistent symptoms after whiplash, may help sufferers to gain early and more suited treatment, which in turn may prevent the condition from becoming chronic.
INTRODUCTION
The development of persistent pain after a whiplash injury is still an unresolved mystery. Although recovery is to be expected within a few weeks [1] about 50% develop persistent symptoms and pain. Common symptoms after whiplash injury are neck pain, headache, shoulder pain, sleep disturbances, fatigue, and cognitive problems. The array of symptoms and pain experienced after whiplash injury are labelled as whiplash associated disorder (WAD). To classify different grades of WAD, the Quebec Task Force [2] has developed a nomenclature classifying whiplash injuries from grade 0-IV. The majority (90%) of whiplash injured patients are classified as grade I-II. Grade I is characterised by neck pain, stiffness, or tenderness only, without any physical signs of injury. Grade II is characterised by additional musculoskeletal signs and a decreased range of motion. It is generally acknowledged that an initial injury occurs to the neck following whiplash trauma. In addition, a number of pheripheral and central mechanisms in the spinal cord and supraspinal nervous centres are found to upregulate the nociceptive processes. What makes WAD a controversial condition is the wide variety in patient responses to seemingly the same extent of physical pathology. Moreover, even though precise identification of injured structures is possible it is doubtful that identification of such structures will improve treatment [3]. However, an additional identification of psychological mechanisms that may interact with the physical injury after whiplash injury would have significant value in guiding early treatment interventions.
There is a general consensus that high initial pain, disability, decreased range of motion, and psychological distress, are indicators of a poor prognosis after whiplash injury [4-7]. In particular, posttraumatic stress symptoms (PTSS) have been associated with pain intensity and poor adjustment after whiplash injury. More recently, attachment insecurity has also been mentioned as a pre-trauma vulnerability factor for both posttraumatic stress [8-11] and the perception of pain [12, 13].
ATTACHMENT INSECURITY AND WHIPLASH
Attachment orientations are shaped from early relationship experiences and thought to be relatively stable schemas through life. They are described as complex internal ‘working models’ of the ‘self’ and ‘others’, which affect the way we perceive threats, regulate emotions, and respond to stressors [14]. Adult attachment orientations can be characterised along two dimensions: attachment anxiety (worry over the availability and positive regard of others) and attachment avoidance (discomfort with closeness and dependence on others). The combinations of the two dimensions define four attachment styles. Individuals with both low levels of attachment anxiety and attachment avoidance are characterised as securely attached. Individuals with high levels of attachment anxiety and low levels of avoidance are characterised as preoccupied (with attachment) and individuals with both high levels of attachment anxiety and avoidance are characterised as fearful. Finally, individuals with low levels of anxiety and high levels of avoidance are characterised as dismissing [15]. Attachment insecurity may contribute to posttraumatic stress, pain, and somatisation in several inter-related ways. Attachment anxiety is associated with hyperactivating strategies such as, catastrophizing, hypervigilance, prolonged emotional distress, and excessive dependence on others [16]. Attachment avoidance is associated with deactivating strategies such as underestimation of threats, avoidance of threat related cues, and underutilising social support [16, 17].
Increasing evidence has linked attachment insecurity to chronic pain conditions [for a review see [13], PTSD (for a review see [16]) and number of somatic symptoms reported in various samples of patient groups and healthy adults [18-21]. In particular, attachment anxiety has been associated with a wider range of health conditions, pain, and somatisation [22,24]. In a review, Meredith and colleagues [13] propose a heuristic model explaining how attachment insecurity may affect the experience of pain via different psychological mediators, such as self appraisals, emotional states and coping strategies. However, the causal mechanisms between attachment insecurity and the experience of pain and somatisation are still an under-investigated area. In particular, deficits in affect regulation and difficulties differentiating emotional arousal from other bodily sensations have often been raised as important mechanism [10, 17, 22-23]. The preoccupied and fearful attachment styles (high attachment anxiety) have both been associated with hypervigilance to interoceptive sensations leading to misinterpreting neutral bodily sensations as a potential threat [21, 24, 25]. Moreover, individuals with high levels of attachment anxiety are believed to be more likely to report somatic symptoms as a consequence of their tendency to focus on negative affect. Conversely, individuals with high levels of attachment avoidance do not focus on negative affect, as a result they tend to underreport somatic symptoms [26]. In a large study of female medical patients (n=701) Ciechanowski and colleagues [21] found that individuals with a preoccupied or fearful attachment style reported significantly more somatic symptoms compared to women with a secure or dismissing attachment style. This association remained significant even after adjusting for concurrent depression. The most robust associations found are often between attachment insecurity and various forms of psychological distress, in particular depression and anxiety disorders, which may mediate the association between attachment, pain, and somatisation [16, 27, 28].
PTSD AND WHIPLASH
In comparing patients with WAD grade I-II who also experience PTSD compared to those with WAD grade I-II who do not experience PTSD, the former report a higher level of pain and more somatic symptoms compared to the latter [19, 22, 29, 30]. The higher level of symptom reporting may be attributed to elevated levels of anxiety and avoidance behaviors. In addition, direct sensitisation to pain (hyperalgesia) may develop as a consequence of the traumatic experience and prolonged distress [19, 30, 31]. In whiplash accidents where pain is part of the trauma, sensitisation to pain may also develop because pain serves as a reminder of the traumatic experience [32]. Recently it has been demonstrated that mutual maintenance of PTSD and persistent pain existed in the early aftermath of an accident [33]. In particular, the severity of hyperarousal symptoms has been associated with the development of persistent symptoms after whiplash [6, 34]. It has also been reported that, even up to 5-years post-injury, PTSD symptom clusters hyperarousal and avoidance have been associated with pain, somatisation, and disability [19].
Furthermore, cognitive and behavioural avoidance of traumatic memories have been linked to increased stress response and somatoform disorders [23]. In a large prospective population study, Andresky and colleagues [35] found that PTSD was the psychiatric disorder most associated with somatisation and medically unexplained pain. In addition, a study of Gulf War veterans, showed that those with PTSD, displayed significantly more physical symptoms compared to controls without PTSD [36]. In particular, hyperarousal symptoms have been associated with physical health concerns [37]. Indeed, even in cases were the PTSD symptoms had resolved, high levels of somatisation were still present. This indicates that PTSD may be part of the aetiology of somatisation, also affecting other mechanisms that maintain somatisation [10].
AIMS AND HYPOTHESES
The present study examined attachment insecurity and PTSD symptoms as possible vulnerability factors in relation to high levels of pain and somatisation after sub-acute whiplash injury.
Hypotheses.
We predicted that the attachment dimensions (avoidance and anxiety) were positively associated with pain, somatisation, and PTSD symptom clusters. In addition, we predicted that the association between the attachment dimensions, pain, and somatisation would be mediated by the PTSD symptom clusters, with hyperarousal being the strongest mediator. Furthermore, we predicted that those fulfilling the DSM-IV criteria for the three PTSD symptom clusters were increasingly at risk of having moderate to severe pain and high levels of somatisation.
METHODS
Participants
A cross-sectional cohort design was used to assess patients after sub-acute whiplash trauma. Data were collected from July 2009 to December 2010. In the time period 327 patients (women = 204) were referred consecutively to the emergency unit after acute whiplash injury. For demographic details see Table 1. All patients had whiplash grade I-III (Quebec task force: [2]). Most had WAD grade I-II (95%). Head injury and unconsciousness as well as other serious injuries lead to exclusion from the study. Within one-month post injury (median 19 days), patients answered a questionnaire regarding attachment, pain, somatisation, depression, and PTSD symptoms. During the intake period, 578 questionnaires were dispatched. Questionnaires were not sent to accident victims under 18 years of age. A total of 327 (57%) initial questionnaires were returned.
Demographic Details and Descriptive Information for Categorical Variables
| Variable | N = 327 | % | |
|---|---|---|---|
|
|
|||
| Age | Mean years | 36.5 | |
| (SD) | (13.7) | ||
|
|
|||
| Gender | Male | 123 | 37.6 |
|
|
|||
| Female | 204 | 62.4 | |
|
|
|||
| Marital status | Single | 79 | 24.2 |
|
|
|||
| Married/de facto | 227 | 69.6 | |
|
|
|||
| Divorced | 18 | 5.5 | |
|
|
|||
| Widowed | 2 | 0.6 | |
|
|
|||
| Education | Basic school mean years | 10.8 | |
| (SD) | (2.3) | ||
|
|
|||
| Further education mean years | 3.7 | ||
| (SD) | (2.5) | ||
|
|
|||
| Current employment | Full time | 137 | 41.9 |
|
|
|||
| Part time | 11 | 3.4 | |
|
|
|||
| Unemployed | 22 | 6.7 | |
|
|
|||
| Retired | 15 | 4.6 | |
|
|
|||
| Student | 60 | 18.3 | |
|
|
|||
| Other | 29 | 8.9 | |
|
|
|||
| Accident | Injured in the traffic | 252 | 77.1 |
|
|
|||
| Other minor injuries | 163 | 49.8 | |
|
|
|||
| Cut-off criteria | PTSD | 49 | 15.0 |
|
|
|||
| Somatisation | 38 | 11.6 | |
|
|
|||
| Moderate-severe pain | VAS mean score > 4.5 | 115 | 35.2 |
|
|
|||
| Pre-injury | Chronic pain | 47 | 14.4 |
Coefficients for the Mediation Models of the Attachment Dimensions on Pain and Somatisation
| Pain | Somatisation | |||
|---|---|---|---|---|
| Attachment-Avoidance | Path a (SE) | Path b (SE) | Path a (SE) | Path b (SE) |
| Mediator | ||||
| Intrusion | 0.08*(.02) | -0.02 (.06) | 0.08*(.02) | -0.33*(.10) |
| Avoidance | 0.20*(.03) | 0.11*(.04) | 0.20*(.03) | 0.37*(.07) |
| Hyperarousal | 0.18*(.03) | 0.26*(.05) | 0.18*(.03) | 0.90*(.07) |
| Attachment-anxiety | ||||
| Mediator | ||||
| Intrusion | 0.15*(.03) | -0.02(.06) | 0.15*(.03) | -0.35*(.09) |
| Avoidance | 0.33*(.04) | 0.13*(.04) | 0.33*(.04) | 0.36*(.07) |
| Hyperarousal | 0.28*(.04) | 0.27*(.05) | 0.28*(.04) | 0.90*(.07) |
Note. SE = standard error
* p < .05.
Indirect Effects (Mediated) of the Attachment Dimensions on Pain and Somatisation
| Pain | Somatisation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Product of Coefficients | BC 95% CI | Product of Coefficients | BC 95% CI | ||||||||
| Attachment-avoidance | Point Estimate | SE | Z | Lower | Upper | Point Estimate | SE | Z | Lower | Upper | |
| Mediator (PTSD) | |||||||||||
| Intrusion | -0.00 | 0.01 | -0.27 | -0.01 | 0.01 | -0.03* | 0.01 | -2.63 | -0.05 | -0.01 | |
| Avoidance | 0.02* | 0.01 | 2.42 | 0.00 | 0.05 | 0.08* | 0.02 | 4.11 | 0.04 | 0.12 | |
| Hyperarousal | 0.05* | 0.01 | 4.30 | 0.03 | 0.07 | 0.16* | 0.03 | 5.79 | 0.11 | 0.22 | |
| Attachment-Anxiety | |||||||||||
| Mediator (PTSD) | |||||||||||
| Intrusion | -0.00 | 0.01 | -0.38 | -0.02 | 0.02 | -0.05* | 0.02 | -2.95 | -0.10 | -0.02 | |
| Avoidance | 0.04* | 0.02 | 2.76 | 0.01 | 0.08 | 0.12* | 0.03 | 4.13 | 0.06 | 0.20 | |
| Hyperarousal | 0,08* | 0.02 | 4.47 | 0.05 | 0.11 | 0.25* | 0.04 | 5.92 | 0.17 | 0.34 | |
Note. SE = standard error; BC = bias corrected; CI = confidence interval.
* p < .05
Multiple Logistic Regression Models for Pain and Somatisation
| Variable | Coefficient (β) | S.E. | Wald χ2 | P value | Odds ratio | 95% CI Lower Upper | |
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Pain | |||||||
|
|
|||||||
| Constant | -1.573 | 0.445 | 12.471 | 0.001 | 0.207 | ||
|
|
|||||||
| Gender | 0.256 | 0.275 | 0.870 | 0.351 | 1.292 | 0.754 | 2.214 |
|
|
|||||||
| Age | 0.007 | 0.010 | 0.471 | 0.493 | 1.007 | 0.988 | 1.026 |
|
|
|||||||
| Depression | 1.597 | 0.332 | 23.183 | 0.001 | 4.939 | 2.578 | 9.462 |
| PTSD | 1.094 | 0.445 | 12.471 | 0.005 | 2.986 | 1.389 | 6.421 |
|
|
|||||||
| Somatisation | |||||||
|
|
|||||||
| Constant | -3.075 | 0.725 | 18.005 | 0.001 | 0.046 | ||
|
|
|||||||
| Gender | -0.986 | 0.433 | 5.188 | 0.023 | 0.373 | 0.160 | 0.872 |
|
|
|||||||
| Age | 0.007 | 0.015 | 0.243 | 0.622 | 1.008 | 0.978 | 1.038 |
|
|
|||||||
| Depression | 2.132 | 0.475 | 20.127 | 0.001 | 8.434 | 3.323 | 21.410 |
|
|
|||||||
| PTSD | 1.316 | 0.474 | 7.696 | 0.006 | 3.727 | 1.471 | 9.441 |
Note. Pain = Mean VAS pain (score ≥ 4.5). Somatisation = Men (symptoms on TSC ≥ 4), women (symptoms on TSC ≥ 6).
Measures
Attachment security was measured with the Revised Adult Attachment Scale (RAAS; [38]). RAAS is an 18-item self-report scale, on which participants rate statements about how they function and feel in a relationship with a partner, someone close, and people in general on a 5-point Likert scale; 1 = not at all characteristic, 5 = very characteristic. The scale is two-dimensional; (1) items on closeness and dependency are merged into one dimension “Avoidance” (α = .78), and (2) an "Anxious" attachment dimension (α = .80). Attachment security is defined by a combined score, below midpoint (< 36) on the avoidance dimension and a score below midpoint (< 18) on the anxious dimension. Attachment insecurity is defined as a combined score, above midpoint (> 36) on the avoidance dimension and/or a score above midpoint (> 18) on the anxious dimension. Cronbach’s alpha for the total scale (α = 85).
The Trauma Symptom Checklist — Revised (TSC-R; [39]) was used to measure somatisation. The somatisation scale consists of 10 items measuring the presence of medically unexplained somatic symptoms on a 4-point Likert scale (1 = never, 4 = always). Cronbach’s alpha for the total scale was = .85. According to the DSM-IV [40] a diagnosis of a somatisation disorder applies to patients with a history of at least eight different medically unexplained symptoms: pain in at least four different sites of the body, two gastrointestinal symptoms, one sexual symptom, and one pseudoneurological symptom. A less restrictive criteria has been used in research i.e., defining somatisation as the endorsement of four somatoform symptoms in men and six in women [35]. The level of somatisation was both measured on a continuum and by the criteria of at least four somatic symptoms for men and six for women. An item was endorsed if the score was ≥ 3.
To measure the severity of PTSD symptomotology we used The Harvard Trauma Questionnaire part IV (HTQ; [41]). The HTQ consists of 16 items on a 4-point Likert scale (1 = not at all, 4 = very often). The items relate to the three core clusters of PTSD in the DSM-IV: avoidance (7 items, α = .83), intrusion (4 items, α = .81), and hyperarousal (5 items, α = .82). Following the DSM-IV, a PTSD diagnosis was proposed if participants reported at least one intrusive symptom, three avoidance symptoms, and two hyperarousal symptoms. An item was deemed to be positively endorsed if the score was ≥ 3. The HTQ self-report measure of PTSD has an 88% concordance rate with interview based estimates of PTSD [41]. The internal consistency, measured by Cronbach’s alpha, was excellent (total α = .92).
Pain intensity was measured as the average score of four visual analogue scales (VAS; [42]). Each scale measured pain intensity on a 10 cm horizontal line ranging from 0 (no pain) to 10 (the worst possible pain). Patients marked their answers on each line corresponding to their pain now, their highest level of pain, their lowest level of pain, and finally their average pain over the past week. Moderate-severe pain vas defined as a mean VAS score > 4.5. Internal consistency measured by Cronbach’s alpha was excellent (α = 93).
To assess the level of depressive symptoms, we used the Hospital Anxiety and Depression Scale (HADS; [43]). The scale consists of 14 items, seven relating to anxiety (HADS-A) and seven to depression (HADS-D), with responses ranging from 0 (no symptoms) to 3 (maximum impairment). In the present study we only used the subscale of depression. A cut-off score of ≥ 8 was used in order to include all possible cases of depression, as suggested by [43]. Internal consistency measured by Cronbach’s alpha was excellent (α = .87).
Statistical Analysis
Prior to data analysis, the data were screened for errors and missing values. The percentage of missing values was small (0.0- 4.9%). The Expectation Maximization algorithm was used to impute missing data [44]. All analyses were conducted in SPSS version 19.0. Multiple mediation analyses were performed using the approach proposed by Preacher and Hayes [45]. This approach has high statistical power which is often raised as a concern when using the Sobels test, unless the sample size is very large. The model was specified and estimated using the Preacher and Hayes [45] macro for SPSS 19 based on maximum likelihood estimation and 5000 bootstrap draws. The analysis estimated the direct effect of the attachment dimensions on pain and somatisation and the indirect effect mediated by the three PTSD symptom clusters. The multiple mediator model is presented in Fig. (1). The following terms are used for the different pathways: the “total effect” is the relationship between the attachment dimensions and pain and somatisation (path c); the “indirect effect” is the effect of the attachment dimensions on pain and somatisation via the mediators (a*b); the “direct effect” is the effect of the attachment dimensions on pain and somatisation adjusted for the mediators (c’). The strength of the mediation is represented as the difference in the estimated path c and path c’. Full mediation is evident when path c is statistically significant, but becomes non-significant after adjusting for the mediators. The percentage mediated by each mediator is calculated as 1- (c’/c).
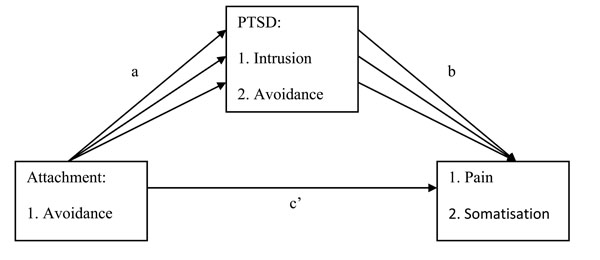
Attachment dimensions, pain, somatisation and mediators.
Note: Four separate models were estimated, a model for each dependent variable (pain and somatisation) with each independent variable (attachment avoidance and anxiety).
Logistic regression was used to determine the likelihood with which participants, who fulfilled the DSM-IV criteria for the three PTSD symptom clusters, would report moderate to severe pain and somatisation according to the cut-off criteria used [35].
RESULTS
Mediation Attachment on Pain
The total effect (c) between both attachment dimensions (avoidance and anxiety) and pain were positive and statistically significant; avoidance (B = .08, S.E. = .02, p < .001), anxiety (B = .08, S.E. = .03, p < .01), with no mediators in the model. When the effects of the mediators were included in the model the direct path (c’) turned non-significant; avoidance (B = .01, S.E. = .02, p > .05), anxiety (B = -.03, S.E. = .02, p > .05 which indicated full mediation. The mediators accounted for 61% of the total effect in relation to attachment anxiety and for 85% in relation to attachment avoidance. The unstandardized estimates for path (a) and path (b) from the mediation models are reported in Table 2. The regression coefficients of the effects of both attachment dimensions on the hypothesised mediators; the PTSD symptom clusters (path a), were all positive and statistically significant. The effects of the mediators on pain (path b) were also positive and statistically significant with the exception of intrusion which was non-significant.
Table 3. shows the indirect effects (a*b) of the attachment dimensions on pain. The indirect effects associated with the mediating variables; the PTSD symptom clusters of avoidance and hyperarousal, were positive and statistically significant. The symptom cluster intrusion was non-significant. Overall, the PSTD symptom cluster hyperarousal was the strongest mediator. Moreover, the largest effects were found between attachment anxiety and the mediators (path a).
Mediation Attachment on Somatisation
The total effect (c) between both attachment dimensions (avoidance and anxiety) and somatisation were positive and statistically significant; avoidance (B = .27, S.E. = .04, p < .001), anxiety (B = .44, S.E. = .06, p < .001), with no mediators in the model. When the effects of the mediators were included in the model the direct path (c’) was reduced, however still significant; avoidance (B = .06, S.E. = .03, p < .05), anxiety (B = .12, S.E. = .04, p < .01 which indicated partial mediation. The mediators accounted for 72% of the total effect in relation to attachment anxiety and for 77% in relation to attachment avoidance. The unstandardized estimates for path (a) and path (b) from the mediation models are reported in Table 2. The regression coefficients of the effects of both attachment dimensions on the hypothesised mediators; the PTSD symptom clusters (path a), were all positive and statistically significant. The effects of the mediators on somatisation (path b) were also statistically significant. However, the effect of intrusion on somatisation was negative.
Table 3. shows the indirect effects (a*b) of the attachment dimensions on somatisation. The indirect effects associated with the mediating variables; the PTSD symptom clusters avoidance and hyperarousal, were positive and statistically significant. The symptom cluster intrusion was also significant but negative. Also in relation to somatisation the PSTD symptom cluster hyperarousal was the strongest mediator.
Logistic Regression. PTSD on Pain and Somatisation
A total of 49 patients (15%) fulfilled the DSM-IV symptom cluster criteria for a possible PTSD diagnosis and 115 patients (35.2%) were endorsed as having moderate-severe pain. Finally, 38 patients (11.6%) fulfilled the criteria [31] for somatisation.
Of the covariates only gender was significantly related to somatisation. Depressive symptoms were significantly related to both pain and somatisation. Fulfilling the DSM-IV PTSD criteria increased the likelihood of belonging to the moderate-severe pain group three-fold. In relation to somatisation the likelihood of belonging to the group was almost increased four-fold. The Odds ratios are reported in Table 4.
DISCUSSION
In agreement with previous studies we found support for the first hypothesis that both attachment dimensions were positively associated with the dependent variables, pain, somatisation, and PTSD symptoms. The strongest association was between attachment anxiety and all the dependent variables. The results are in agreement with Meredith et al. [12], who found that attachment anxiety was causally related to pain catastrophizing and low pain thresholds. However, the strongest associations were between attachment anxiety, PTSD symptoms, and somatisation. This is also in agreement with previous studies that have often found significant but small direct correlations between attachment and pain and more robust associations between attachment insecurity and somatisation [18] and psychological distress [13]. In particular, attachment-anxiety was associated with high levels of PTSD hyperarousal and avoidance, which in turn fully mediated the relationship between attachment-anxiety and pain. The results are in accordance with the shared vulnerability model [11] proposing anxiety as a vulnerability factor lowering the physiological threshold for fight/flight responses. This finding is only partially in alignment with Waller et al. [23] who found that most patients with a somatisation disorder were avoidant attached.
The second hypothesis regarding mediation was confirmed. However, there were no significant associations between the PTSD symptom cluster intrusion and pain (path b) and the association between intrusion and somatisation was negative. This finding is contrary to what was expected, i.e., that pain would be associated with the trauma and thus would activate intrusive memories about the traumatic event [32].
In agreement with earlier findings, the present study also indicates that attachment insecurity may be a diathesis for problematic adjustment to pain. The attachment dimensions seem to contribute to the experience of pain and somatisation by triggering different cognitive, behavioural, and emotional regulatory mechanisms. Identifying some of these possible mechanisms maintaining elevated levels of pain and somatisation after whiplash injury may have important clinical implications for treatment planning.
It is reasonable to assume that attachment-anxiety contributes to the experience of pain and somatisation via elevated levels of arousal and muscle tension, which is known to worsen pain. Also, elevated levels of PTSD hyperarousal may increase anxiety, leading to muscle tension and avoidance behavior which maintains and exacerbates the pain condition. Moreover, negative affect may be an important general vulnerability factor exacerbated by attachment anxiety. Finally, attachment-avoidance may contribute negatively to adjustment after whiplash injury by increasing both PTSD and pain avoidance behavior [11, 16].
The strongest mediator between both the attachment dimensions, and pain and somatisation was hyperarousal symptoms. This finding is in agreement with Buitenhuis et al. [6] and Liedl et al. [34] who found that hyperarousal symptoms within 1-month post injury were the most important risk factor for persistent whiplash symptoms at 6- and 12-months post injury. The robustness of hyperarousal symptoms as important risk factors, were further supported by Andersen et al. [19], who found that the severity of hyperaroual symptoms were strongly related to pain, somatisation, and whiplash symptoms, more than 5-years after the whiplash injury. The third hypothesis was also confirmed. In agreement with other studies, PTSD was an important predictor of both pain [5, 6] and somatisation [35]. However, the level of depressive symptoms was the single best predictor of pain and somatisation.
It is still debateable whether attachment insecurity is a pre-trauma vulnerability factor affecting the perception and development of pain or whether the traumatic experience and the pain condition, in-itself, increases attachment insecurity. However, in a recent experimental setting it was found that attachment anxiety measured prior to a coldpressor task was associated with lower pain thresholds, stress and pain catastrophizing [12]. It is important to highlight that it is unlikely that a whiplash injury affects the attachment orientation within a few short weeks. Also, in a recent study, it was found that motor vehicle accidents did not affect attachment orientations as only interpersonal traumas had an impact [46].
Limitations and Strengths
The present study has several limitations. The first being, that the results are based on cross-sectional data only. Secondly, since patients were included early after their injury (median time 19 days) it is most possible that a substantial number recover spontaneously within the following weeks. Hence, it is not possible to make any strong predictions about the risk of developing persistent symptoms. Although attachment orientations are thought to be relatively stable traits, truly investigating attachment insecurity as a vulnerability factor requires a longitudinal design, which measures attachment prior to the accident. Another limitation is the response rate. It is possible that the response may be biased toward those representing the least symptomatic cohort as those may be the individuals who return the questionnaire. However, we found no differences between responders and non-responders regarding gender, age and WAD grade. Compared to other studies we would have expected a higher prevalence of possible PTSD cases. Furthermore, the level of attachment insecurity was low compared to the general population. The use of self report measures is a further limitation. Finally, given the acute state one could also argue that a measure of acute stress disorder would be more appropriate. However, the aim of the present study was to investigate the mediating role of the PTSD symptom clusters in relation to somatisation and pain after sub-acute whiplash injury. Despite these limitations the present study has several strengths. A major strength is that the data represents a total cohort of consecutive whiplash patients referred to a large Danish emergency room. Moreover, all patients were carefully screened for whiplash grade at the initial contact with the physician. Also the use of mediation analysis gives more detailed knowledge about interacting mechanisms.
CONCLUSION
With PTSD symptoms and somatisation representing important features of the whiplash associated disorder, traditional pain management may miss important features. Clinicians may be misguided in their interventions, because patients with symptoms of whiplash, may primarily seek treatment for pain complaints. In relation to affect regulation, factors such as PTSD, somatisation, and attachment insecurity may be overlooked despite being highlighted as potential vulnerabilities. Indeed, cognitive behavioural therapy has been found effective for many PTSD sufferers [47], however when the trauma is associated with persistent pain less improvement is found [48]. Thus, when treating whiplash patients for PTSD, the clinician may need to target hyperarousal and avoidance symptoms to a larger extent than intrusive memories. Other problems associated with PTSD, such as affect dysregulation (high attachment-anxiety), dissociation, somatisation, and difficulties with trust and intimacy (attachment-avoidance) may also maintain the two conditions; this is why they should be addressed in treatment. Persistent symptoms after whiplash injury are often characterised as medically unexplained symptoms leading to stigmatisation by not acknowledging the pain as “real” pain but pain with a psychological origin. Acknowledging that PTSD is part of the aetiology, involved in explaining persistent symptoms after whiplash trauma, may help sufferers to gain early and more suited treatment which in turn may prevent the condition from becoming chronic.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
We would like to thank the Danish Society for Polio, Traffic, and Accident Victims and its members for their support in the present study. In addition, we would like to extend our gratitude to Allevia - Multidisciplinary Pain Centre, Denmark for their support.


