All published articles of this journal are available on ScienceDirect.
Functional Remediation for Bipolar Disorder
Abstract
Neurocognitive impairment constitutes a core feature of bipolar illness. The main domains affected are verbal memory, attention, and executive functions. Deficits in these areas as well as difficulties to get functional remission seem to be increased associated with illness progression. Several studies have found a strong relationship between neurocognitive impairment and low functioning in bipolar disorder, as previously reported in other illnesses such as schizophrenia. Cognitive remediation strategies, adapted from work conducted with traumatic brain injury patients and applied to patients with schizophrenia, also need to be adapted to individuals with bipolar disorders. Early intervention using functional remediation, involves neurocognitive techniques and training, but also psychoeducation on cognition-related issues and problem-solving within an ecological framework.
INTRODUCTION
The term “functional remediation” refers to interventions aimed at restoring psychosocial functioning in patients with brain disorders, including, obviously, mental disorders, by means of ecological neurocognitive techniques. The term “ecological” tries to emphasize the practical effectiveness of those interventions on daily life, as opposed to other, which may be criticised as of being closer to “brain training” rather than real functioning. Functional remediation involves psychoeducation about cognitive dysfunctions and their impact on the general functioning.
NEUROCOGNITIVE IMPAIRMENT IN BIPOLAR DISORDER
In the last decade we have seen that cognitive impairment is a core feature of bipolar illness. Cognitive deficits persist during euthymia and may include attention, executive function, and verbal memory impairment [1-5]. These cognitive dysfunctions may reflect abnormal activation patterns in the brain [6, 7], involving the prefrontal cortex in the etiopathogenesis of bipolar illness and positing cortical-subcortical-limbic disruption as the underlying cause [8, 9]. Such deficits do not seem to be specific and their pattern is quite similar to schizophrenia, albeit overall less severe [10, 11]. Euthymic bipolar patients demonstrate relatively marked impairment in aspects of executive function and verbal memory [1]. It is not clear yet whether these are two discrete areas of impairment or whether such deficits are related one to another. In addition, is yet to be determined whether neuropsychological impairment is already present before the clinical onset of the disorder, although several studies suggest that bipolar patients may be relatively preserved from the neurocognitive point of view before developing their condition. Several studies have looked in different ways at the cognitive performance of large cohorts of children or youth and analyzed the specific profile of those who would subsequently develop bipolar disorder or schizophrenia; overall, there is no suggestion for severe deficits prior to onset of bipolar disorder, whereas there seems to be so for schizophrenia [12-14] perhaps with the exception of visuospatial reasoning [15]. Interestingly, subjects at risk for bipolar disorder were more likely than subjects at risk for schizophrenia and even than subjects at no risk for mental disorders to perform better in some domains [14], particularly at arithmetic reasoning [15]. Neuropsychological studies on first-degree relatives of subjects with bipolar disorder, though, suggest that there might be some mild deficits underlying vulnerability to the disorder in the areas of psychomotor speed and executive function [16-18], but not verbal memory [19]. In fact, verbal memory was not found to be related to increased risk for bipolar disorder in premorbid neuropsychological studies [15], but seems to be strongly affected by the impact of multiple episodes [3], subthreshold depressive symptoms [20], and medication [21-24]. Hence, verbal memory may be a potential treatment target by means of effective prophylactic treatment, improvement of subclinical depressive symptoms, and rational use of medication. Importantly, verbal memory performance has been reported to be highly correlated with functional outcome [25-27].
Neurocognitive impairment may not occur exclusively in individuals with bipolar type I disorder, as it has been reported in bipolar II disorder [28], schizoaffective disorder bipolar type [29], bipolar patients with and without history of psychosis [22, 30, 31], bipolar suicide attempters [32], bipolar patients with comorbid conditions [33-35], and pediatric bipolar disorder [36]. On the other hand, a subset of bipolar patients seems to have little or no cognitive impairment [37]. In general, between 40% and 60% of bipolar patients show neurocognitive deficits in early phases of the illness [38] and deficits are more marked in those patients with more relapses [39]. Thus, the study of bipolar subtypes and subgroups, including those who do not show cognitive deficits, may provide important clues for the effective treatment and prevention of cognitive impairment and psychosocial dysfunction.
IMPACT OF NEUROCOGNITIVE IMPAIRMENT ON FUNCTIONING
There is an increasing evidence of a relationship between cognitive impairment and low functioning in bipolar patients. The experience in schizophrenic patients can help to clear that neurocognitive functioning may be more strongly associated with functional outcome than clinical symptoms. In this case, and especially during the last decade, several studies have pointed out to the correlation between the performance on specific cognitive tasks and lower psychosocial functioning assessed through general measures, such as the GAF [40]. Most of these studies tried to control for the impact of subclinical symptoms that have been considered as a negative influence for the functional recovery of bipolar patients. One of the main problems is that remission and euthymia criteria are often not clearly defined, so differences between studies were found [41].
In recent studies, an association between CVLT verbal memory measures and low functioning was consistently found [3, 27, 42, 43]. Poor planning and problem solving were associated with functioning, so that difficulties with logical approaches to problems in daily living may have the greatest impact in functional outcome [44]. Other executive function measures correlated with social disability, but weakly [45]. TMT-B was also found to be a good correlate of functioning in bipolar I and II patients [28]. Recent publications also reported that executive function performance was related to employment status [46]. Moreover, a connection between the RBANS immediate memory performance and the current work status was also reported [47].
Jaeger and Vieta [48] co-edited a special issue on functionality in Bipolar Disorders, including four studies linking cognition and functioning. WCST categories correlated with GAF scores [49]. Dittmann et al. [50] reported that psychosocial functioning was significantly correlated with working memory measures. Martinez-Aran et al. [25] found that CVLT verbal recall was the measure that best predicted psychosocial functioning. Finally, Jaeger et al. [51] looked for predictors of functional remission one year after discharge due to an acute episode. Attention and ideational fluency were the factors that best predicted functioning. In this line, another study showed that the Neurocognitive Global Index and, specifically, speed of processing were the best predictors of functional remission at one-year follow-up [52]. Persistent deficits in verbal memory, executive functions and attention may lead to impairments in occupational, social and interpersonal functioning, so we should optimize not only cognitive but also functional measures. There are very few longitudinal studies focused on the analysis of predictive factors of functioning in bipolar disorder. Discrepancies on the findings from different studies emphasize the need for consensus on the assessment of bipolar patients. The development of core-sets for bipolar disorder, based on the International Classification of Functioning, Disability and Health (ICF), may be useful in further research [53]. The ISBD-BANC is promoting a consensus battery for the neurocognitive assessment of bipolar patients as well [54]. Moreover, the use of brief instruments focused on specific functional areas affected in bipolar patients, will allow identify correlates of different areas of functioning [55]. The cognitive measures found to be associated with functioning vary between studies and, in general, they have not been found to be strongly correlated. Findings seem to be quite consistent with regard to the relevance of verbal learning and memory measures, such as the California Verbal Learning Test on disability, using the FAST, in longer longitudinal studies [27]. Interestingly, recent findings suggest that executive function measures may also play an essential role on functioning and disability [56]. In this regard, Murray et al. [57] have focused on specific self-management strategies used by high functioning individuals with bipolar disorder in order to maintain or regain wellness, including sleep, diet, rest and exercise, ongoing monitoring, reflective and meditative practices, understanding bipolar disorder and educating others, connecting to others and enacting a plan to prevent relapses. These findings suggest that patients receiving psychoeducation may be more likely to achieve functional recovery [58, 59]. A combination of psychoeducation and functional remediation may be helpful to foster recovery in these patients, taking into account that a neurodegenerative process can lead to poorer functioning in the long-term (see Fig. 1).
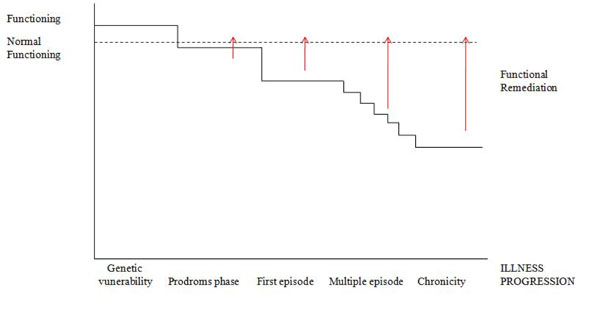
Functional remediation tries to cover the gap between normal functioning and low functioning associated with illness progression. Functioning probably would be higher before illness onset, and some mild difficulties would be appreciated in the prodromal phase. Moderate difficulties in functioning are observed after the first manic episode since patients get clinical remission but most of them do not achieve premorbid functional recovery. A higher number of relapses would have a negative impact on the general functioning of bipolar patients.
COGNITIVE REMEDIATION VERSUS FUNCTIONAL REMEDIATION
Cognitive remediation (CR) has been extensively used for patients with schizophrenia and psychosis. Nevertheless, to our knowledge, there are only five CR studies including affective, bipolar and unipolar, patients [60-64] but only one of them was focused on bipolar patients [60], in other two studies the number of bipolar patients included were not specified [65, 66]. The sample size of these studies ranges from 2 to 18 patients, which is really small, and the duration of interventions goes from 8 to 48 weeks. In general, CR programmes have used cognitive measures pre and post intervention to assess the efficacy of the intervention. More recently, CR has moved beyond cognitive enhancement, trying to reduce disability and improve functioning. McGurk et al. [67] reported that effects of CR on psychosocial functioning were significantly stronger in studies that also provided psychiatric rehabilitation.
Functional remediation (FR) covers not only cognition but also functioning, including psychoeducation about cognitive deficits and their impact on daily life, providing strategies to manage cognitive deficiencies in different cognitive domains, mainly in attention, memory and executive functions. Family is involved in the process to facilitate practice of strategies and reinforcement. In the context of the Barcelona Bipolar Disorder Programme [68], the FR programme for bipolar disorder has been developed, consisting in 21 weekly sessions of 90 minutes of duration that includes 3 sessions of psychoeducation, 2 sessions to improve attention in everyday situations, 6 sessions focused on techniques and strategies to manage memory deficits and 5 more addressed to executive dysfunctions, especially problem solving, time management, planning and establishing priorities. Sessions are practical including daily life examples, individual and group tasks, role-playings and taking home practical exercises. The remaining sessions are related to improve communication and interpersonal relationships, autonomy and stress management. The effectiveness of the programme is assessed not only through a comprehensive neuropsychological battery but also through measures of functionality, disability, and quality of life, such as the FAST, WHO-DAS-II and SF-36. These tools help us to establish the nature of the problems, and to analyse changes selecting, as outcome variable, the FAST [55, 69]. Clearly, we do not try to just treat the inability to perform a particular neurocognitive test, since an improvement on such a test is not the best way of measuring real-life outcomes [70].
A neuro-cognitive-behavioral approach has been taken into consideration in order to plan this FR programme addressed to bipolar disorder, so that, modelling techniques, role-playing, verbal instructions, self-instructions, positive reinforcement and meta-cognitive cues, among others, have been included. We need to combine theories, methodologies and approaches in order to enhance not only cognition but also functioning in these patients due to the complexity and severity of bipolar disorder, but especially to prevent or reduce neuroprogression.
CONCLUSIONS
Although cognitive rehabilitation is currently being explored in an attempt to improve the neurocognitive performance of schizophrenic as well as bipolar patients, and ultimately their functional outcome, we have coined the term “functional remediation” to define an innovative strategy aimed at targeting the critical factors for full psychosocial adjustment and functional recovery in the context of psychoses and, more specifically, manic-depressive illness. Functional remediation involves neurocognitive techniques and training, but also psychoeducation on cognition-related issues and problem-solving within an ecological framework. The inclusion of context processing, performance monitoring, encoding and manipulation of the information as well as foster compensatory strategies must be included in the FR intervention. In this regard, real-world problems affecting daily functioning are used in FR for bipolar disorder to be transferred to daily practice. A clinical trial assessing the effectiveness of this strategy is on the way, using as primary outcome a functionality measure.


