All published articles of this journal are available on ScienceDirect.
The Role of Family Variables in the Length of Stay of Psychiatric In-patients
Abstract
Background:
In Japan, the number of beds and average length of stay in a psychiatric ward are greater than in other developed countries.
Objective:
The present study aimed to investigate the association between family variables and the length of stay of patients with mental and behavioural disorders in a private psychiatric hospital in Japan.
Methods:
The medical records of patients discharged during a one-year period (n=56: men 50.0% excepting 27 patients discharged due to death were re-examined regarding age, laundry type (self-washing of clothes, family washing or supplier washing), number of family visits per one month while hospitalised, and family structure prior to hospitalisation. A length of stay greater than six months was considered the cut-off point for a long hospital stay. Bivariate logistic regression analyses were conducted to identify factors independently associated with the length of stay, adjusted for sex, age, and mental and/or behavioural disorders according to the criteria of the International Statistical Classification of Diseases and Related Health Problems.
Results:
The bivariate-adjusted odds ratio (95% confidence intervals) for in-patients hospitalised for more than six months was 0.08 (0.01, 0.48) for those who used family washing (p = 0.006) compared with those who used supplier washing. The number of visits per month and family structures before hospitalisation were not significantly associated.
Conclusion:
These results suggest that within a private psychiatric hospital in Japan, family washing is associated with shortened stays and frequency of family visits, while family structure is not associated with these factors.
INTRODUCTION
Since 1960, the rate of psychiatric beds per 100,000 residents has decreased in OECD countries due to de-institutional policies and the advent of community care support systems. Conversely, in Japan, the psychiatric bed rates have increased [1-3]. The average length of hospitalisation within a psychiatric ward in 2012 was 298.1 days. While this length is shorter when compared to 1998 (496 days) [1-3], it is still too long. A national patient survey in 2005, observed that ‘social hospitalisation’, which includes baseless hospital care after a patient has become stable, accounted for 70,000 in-patients, of which about 30% were discharged less than one year after admission and about 70% were discharged after one year [2]. The national patient surveys from 1999 and 2002 revealed that nearly 35,000 patients were discharged within these three years [2-4]. Thereafter, about 63,000 patients were newly-admitted and as a result, the number of social hospitalisations virtually did not change [2].
The risk factors associated with long-stay hospitalisation in psychiatric hospitals in Japan include diagnoses of dementia, mental retardation, and schizophrenia, and being men, and older [5, 6]. A long stay can directly cause problems regarding a family’s acceptance, poor improvement of symptoms, and poor recovery of daily living abilities [7].
The present study was conducted to investigate how the length of a patient’s mental health hospitalisation is related to family structure, frequency of visits, and laundry types (self-washing, family washing, supplier washing), which is related to ADL. Our hypotheses were that short-stay admission would be related to living with either a partner or family members, to a high frequency of visits, and/or to self-washing.
MATERIAL AND METHODS
Patients
The present study included a re-examination of the medical records of 83 patients discharged between 1 July 2013 and 30 June 2014, and the collection of data about their age, laundry type (self-washing, family washing, and supplier washing), family visits per month, and family structure prior to hospitalisation. Fifty-six patients (men 50.0%, excepting 27 patients discharged due to death) were included in these data. A diagnosis of a mental and/or behavioural disorder was made by mental health specialists according to the ICD-10. All patients received psychotherapy, occupational therapy, and pharmacological interventions as clinically indicated.
Statistical Analyses
Patients discharged between 2013 and 2014 were divided into three admission durations (under six months, between six months and 20 years, and over 20 years). The following disorder categories of the ICD-10 were used: F00-F09 (organic, including symptomatic, mental disorders), F10-F19 (mental and behavioural disorders due to psychoactive substance use), F20-F29 (schizophrenia, schizotypal and delusional disorders), F30-F39 (mood disorders), and ‘other’ (mental and behavioural disorders except for F00-F09, F10-F19, F20-F29, and F30-F39). The main independent variables of interest were hospitalisation for medical care and protection, laundry type (self-washing, family washing, and supplier washing), family visits per month, and family structure prior to hospitalisation (living with a parent, with a partner, with a son/daughter/brother, alone, in a care facility, or in a medical hospital). These variables were calculated and compared using χ2 tests.
We used log-transformed values for admission duration and family visits per month to account for their skewed distribution. A length of stay of more than six months was considered the cut-off point for a long hospital stay. Bivariate logistic regression analyses were conducted to identify factors independently associated with the length of stay. Odds Ratios were adjusted for age (continuous), sex, and main mental disorder (F00-F09, F10-F19, F20-F29, F30-F39, and ‘others’). Statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS version 22.0; IBM Corp, Tokyo, Japan). Significance was determined at p < 0 .05.
Ethical Considerations
Ethics approval was obtained from five ethics committees of the hospital’s institutional review board. Due to the non-interventional; retrospective design, no informed consent was required; it was waived by the hospital’s institutional review board.
RESULTS
Table 1 shows the characteristics of the patients discharged during the study period, separated by length of stay at discharge. The mean age for patients hospitalised between six months and 20 years was 77.1±11.7 years, which is nearly 10 years older than those in the other admission groups (p = 0.040). In terms of the main mental disorder, F00-F09, F10-F19, and F20-F29 were the most common categories for those hospitalised between six months and 20 years (10.7%, 5.4%, and 17.9%, respectively). F30-F39 was the most common category for those hospitalised for less than six months (7.1%; p < 0.001). Regarding laundry type, self-washing was the most common method for those hospitalised for over 20 years, family washing was most common for those hospitalised for less than six months, and supplier washing was most common for those hospitalised for between six months and 20 years (p < 0.001). The bivariate-adjusted odds ratios (95% confidence intervals) for in-patients hospitalised for more than six months was 0.08 (0.01, 0.48) for family washing (p = 0.006) compared with those who used supplier washing. The number of visits per month and family structures before hospitalisation were not significantly associated (Table 2).
| Admission duration | |||||||
|---|---|---|---|---|---|---|---|
| < 6 month | 6 month ≤, < 20 year | 20 year ≤ | |||||
| Mean | SD | Mean | SD | Mean | SD | p value | |
| n | 17 | 25 | 14 | ||||
| Men (%)a | 52.9 | 36.0 | 71.4 | 0.101 | |||
| Age (year) | 61.5 | 16.0 | 77.1 | 11.7 | 62.9 | 10.5 | 0.040 |
| Hospitalization for medical care and protection (%)a | 94.1 | 88.0 | 71.4 | 0.181 | |||
| Main mental disorder (%)a | 0.007 | ||||||
| F00-F09 | 7.8 | 10.7 | 1.8 | ||||
| F10-F19 | 3.6 | 5.4 | 5.4 | ||||
| F20-F29 | 10.7 | 17.9 | 10.7 | ||||
| F30-F39 | 7.1 | 3.6 | 3.6 | ||||
| Others | 1.8 | 7.1 | 3.6 | ||||
| Laundry type (%)a | <0.001 | ||||||
| Oneself washing | 8.9 | 0.0 | 16.1 | ||||
| Family washing | 16.1 | 7.1 | 0.0 | ||||
| Supplier washing | 5.4 | 37.5 | 8.9 | ||||
| The number of visit per a month (time) | 20.9 | 19.5 | 28.8 | 23.2 | 6.0 | 5.1 | 0.001 |
| Family structure before hospitaliation (%)a | 0.773 | ||||||
| With parent | 10.7 | 17.9 | 10.7 | ||||
| With partner | 7.1 | 3.6 | 3.6 | ||||
| With son or daughter or brother | 7.1 | 10.7 | 1.8 | ||||
| Alone | 3.6 | 5.4 | 5.4 | ||||
| From care facility or medical hospital | 1.8 | 7.1 | 3.6 | ||||
DISCUSSION
The present study evaluated how length of hospitalisation was related to family variables (family visits per month and living situation prior to hospitalisation) and laundry type, which is related to ADL, among in-patients with mental and behavioural disorders in a private psychiatric hospital in Japan. Our results revealed that family washing was related to a reduction in the length of the patients’ hospital stays.
In 1961, when Japan introduced the universal public insurance system, psychiatric hospitals began to increase in number. Furthermore, psychiatric residents began moving from home care to hospital care [8-10]. Although the number of psychiatric beds has decreased in recent years, the number of private hospitals with mental health wards is still high [1-3], constituting about 80% of psychiatric hospitals in Japan. Therefore, it is difficult to reduce the number of psychiatric beds [8-10]. Gigantesco, de Girolamo, Santone Miglio and Picard reported that being in a private psychiatric hospital is also a barrier to discharge in Italy [11]. In addition, mental illness is still strongly stigmatised in Japan [12]. Thus, psychiatric medical care has not sufficiently shifted from hospitalisation back to community care [1-3].
| Un-adjusted- | Adjusted-a | |||||||
|---|---|---|---|---|---|---|---|---|
| Odd ratios | 95% CI | p value | Odd ratios | 95% CI | p value | |||
| Main mental disorder | ||||||||
| F00-F09 | 2.40 | 0.26 | 22.10 | 0.440 | 2.30 | 0.20 | 26.12 | 0.502 |
| F10-F19 | 0.25 | 0.01 | 4.73 | 0.355 | 0.54 | 0.02 | 18.13 | 0.729 |
| F20-F29 | 3.17 | 0.36 | 27.57 | 0.297 | 12.73 | 0.89 | 182.49 | 0.061 |
| F30-F39 | 4.00 | 0.21 | 75.66 | 0.355 | 9.28 | 0.34 | 250.34 | 0.185 |
| Others | 1.00 | 1.00 | ||||||
| Laundry type | ||||||||
| Self washing | 0.29 | 0.06 | 1.32 | 0.108 | 0.76 | 0.09 | 6.84 | 0.810 |
| Family washing | 0.07 | 0.01 | 0.35 | 0.001 | 0.08 | 0.01 | 0.48 | 0.006 |
| Supplier washing | 1.00 | 1.00 | ||||||
| Number of visits per a month (time) | ||||||||
| 0-15 | 3.00 | 0.25 | 36.32 | 0.388 | 0.60 | 0.02 | 14.60 | 0.755 |
| 16-30 | 1.07 | 0.13 | 8.98 | 0.949 | 1.03 | 0.06 | 18.66 | 0.983 |
| 31-45 | 0.48 | 0.09 | 2.42 | 0.371 | 0.27 | 0.03 | 2.53 | 0.254 |
| 46-60 | 1.29 | 0.20 | 8.43 | 0.793 | 0.49 | 0.04 | 5.94 | 0.578 |
| 60 < | 1.00 | 1.00 | ||||||
| Family structure before hospitalization (%) | ||||||||
| With parent | 0.36 | 0.04 | 3.56 | 0.380 | 0.17 | 0.01 | 5.07 | 0.304 |
| With partner | 0.17 | 0.01 | 2.09 | 0.165 | 0.09 | 0.00 | 3.50 | 0.196 |
| With son or daughter or brother | 0.29 | 0.03 | 3.37 | 0.324 | 0.07 | 0.00 | 1.97 | 0.118 |
| Alone | 0.50 | 0.04 | 7.10 | 0.609 | 0.13 | 0.00 | 5.03 | 0.270 |
| From care facility or medical hospital | 1.00 | 1.00 | ||||||
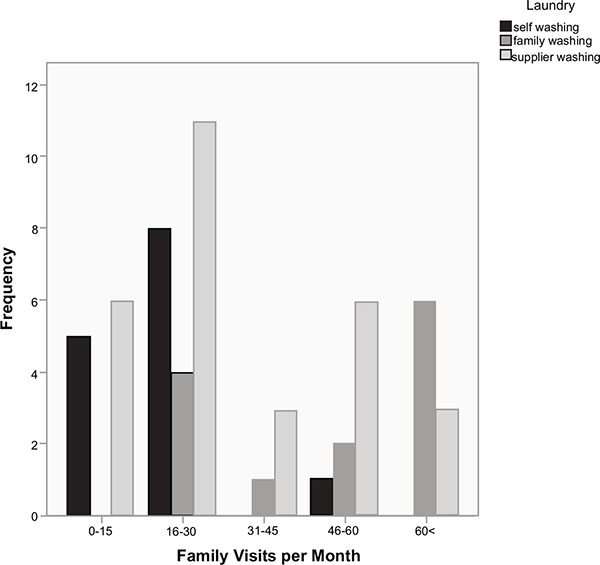
In terms of the relationship between laundry type and visit frequency per months, family washing was observed to be at its highest peak for more than 60 visits per month, and supplier washing was observed to have two high peaks at 16-30 visits and over 46-60 visits (Fig. 1).
In a conventional survey, it was found that patients with dementia, mental retardation, and schizophrenia tended to experience long-stay hospitalisation [5-7]. In the present study, diagnostic status did not significantly influence the length of stay. Likewise in Italy, no difference of diagnostic status emerged between long-stay and short-stay patients [11]. Kawano et al. outlined various factors that relate to a long psychiatric hospitalization including ‘being received by the family’ (51.5%), ‘no symptom improvement’ (48.8%), and ’limited life skills’ (44.0%), whereas for dementia ‘physical diseases’ (20.8%), and ‘no reliable administrative services’ (29.2%) account for longer stays [7].
We assumed that the patient who chooses self-washing will have a short-length of stay because they have somewhat higher to ADL. The results showed that self-washing did not reduce the length of stay, but family washing was related to a short length of stay. Moriyama, et al. conducted a follow-up investigation regarding social hospitalisation processes, which included patient, family, and medical worker interviews [13-15]. The factors relevant to patients were ‘economy’, ’physical functioning’, and the ‘home environment’. The factors relevant to the family were ‘health maintaining the health of the caregiver’, ‘the patient does not apply for certification of the need for long-term care and has received help from home-visit nursing, a home care worker, or a long-term care health facility’, and ‘caregiver burden’. The factor relevant to hospitals was the ‘economic condition of the hospital’. In other words, if beds are not full, the hospital’s profit decreases, affecting the hospitalization-discharge cycle. Thus, if family members intentionally or unintentionally visit when a doctor or chief nurse is absent, the opportunity for discharge and communicative care is diminished. In the present study, if the family was helping with the laundry, the family visited the hospital every two or three days. As such, the opportunity to discuss treatment with hospital staff was more frequent, increasing the probability of earlier discharge. Although one of our hypotheses was that a high frequency of visits would be related to a short length of stay, the frequency of visits was not related to a short length of stay in the present study. However the highest visit frequency occurred if the family was doing the laundry. Conversely, if a supplier was doing the laundry, there were separate peaks during high visit frequencies (Fig. 1). Most supplier washing occurred for patients hospitalised for between six months and 20 years.
The ratio of patients with a diagnosis of F00-F09 was highest in those hospitalised for between six months and 20 years (Table 1). Discharging someone to home care is reasonable for individuals with mild dementia; however, discharge to a care facility is most likely when a patient suffers from severe dementia [16]. This is also the case with other mental disorders (i.e., F10-F19, F20-F29, and F30-F39) [17]. In addition, in the present study, illness severity affected the length of stay. Another of our hypotheses was that self-washing would be related to a short length of stay. Self-washing had a ratio high for the F20-F29 category (Table 1), and severity of disease affected the length of stay. It has been previously reported that family members with high care efficacy [18, 19] and sufficient economic resources [20] are best able to handle a home discharge for individuals with more severe mental health issues.
Another of our hypotheses was that living with a partner or family before hospitalization would be related to a short length of stay. As the present study showed family structure before hospitalisation was not significantly related to reduced hospital stays. Having no children at home increases the length of stay [21]. Tortnicroft, Bebbington, and Leff reported that medical staff tend to carefully discharge a patient into the home environment in Italy because the severity of psychopathology had influenced the length of stay [11]. They showed that improvements in social networks and a less restrictive social environment promote the discharge to the community from a hospital [22, 23]. Thus, we consider that long-stay patients who are discharged from hospital should be supported to live in the community in OECD countries. In 2015 the Ministry of Health, Labour and Welfare reported avenues of reform regarding mental health and medical care welfare [8]. In Japan community-based mental health services have just begun [13]. The main premise is to shift individuals from hospitalisation to community care as a way to recognise and strengthen the medical health care system over the next 10 years [8].
Individuals over the age of 65 years within psychiatric wards accounted for 29% of the patient population in 1996 [4]. This rate increased to 48% in 2008 [4]. Since Japan’s population of individuals over 65 years of age continues to increase [8], further increases in disorders (i.e., dementia) associated with this age group will be likely to occur [3]. In the present study, the private hospital has seen an increase in the number of dementia in-patients in recent years (no data). Thus, there will probably be an increase in the number of in-patients requiring long-term hospitalisation. We need to have close communications and to encourage the discharge of patients.
The present study has several limitations. First, the family’s economic data were not available. It needs to be determined whether family washing is the result of economic concerns or if it is motivated more by the social and psychological benefits for the patient. Second, we did not assess family care efficacy, it could be the case that care efficacy is directly related to family washing behaviour and/or frequency of family visits. Finally, the present study did not assess a patient’s number of a prior social hospitalisations. Further studies are needed to assess how social hospitalisations are related to the variables of interest in the present study.
CONCLUSION
In conclusion, knowing the in-patient family environments helps to encourage discharge and to provide proper care after discharge. The present study indicated that family washing could be an important factor for decreasing the length of stay. In Japan, there are still many private psychiatric hospitals. Furthermore, Japan has become an aging society in recent years. The number of dementia cases is increasing in these psychiatric hospitals, which causes long hospitalisation. In view of this situation further interventional studies should be conducted to investigate the relationship between discharge and communication between in-patients, their families, and hospital staff, and how we are able to help with medical treatment and care.
LIST OF ABBREVIATIONS
| ADL | = Activities of daily living |
| ICD-10 | = International statistical classification of diseases and related health problems |
| OECD | = Organisation for economic cooperation and development |
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Designed the research: SY and YM. Performed the research: SY, YM, KM, KK, EY, SM, YN, and KM. Contributed important reagents: SY, YM, KM, KK, EY, SM, YN, YK and KM. Collected data: SY, YM, KM, KK, EY, SM, YN, and KM. .Analyzed the data: SY and YM. Wrote the paper: SY.


